Introduction
Home care services form part of a broader spectrum of social care services that provide support for people with physical and/or cognitive conditions. While definitions vary, home care typically encompasses support with a range of personal care and essential domestic tasks (Murphy et al. Reference Murphy, Whelan and Normand2015). Most home care is provided by family members and unpaid carers (Maplethorpe et al. Reference Maplethorpe, Darton and Wittenberg2014; Vlachantoni et al. Reference Vlachantoni, Evandrou, Falkingham and Qin2024). Care services are also provided by formal statutory (public) sources (e.g. local authorities) or formal paid sources (e.g. private sector) (Vlachantoni et al. Reference Vlachantoni, Evandrou, Falkingham and Qin2024). In England, around 25.8 per cent of formal care service users use self-funded services and 74.2 per cent use publicly financed services (John Reference John2022).
The high cost and often limited public funding for home care services can have important impacts on adults requiring care, as well as on their families and care-givers: it may result in unmet need for support services, in gaps in the support that is provided, in increased financial strain for the individual and their families if they pay for these services out-of-pocket and/or in reduced labour market participation owing to the need for family or friends to provide informal care (Dunatchik et al. Reference Dunatchik, Icardi, Roberts and Blake2016; Pickard et al. Reference Pickard, King, Brimblecombe and Knapp2018). Understanding how best to support adults with care needs to live at home with dignity and independence for as long as possible is a health policy issue of growing significance.
In 2015, landmark social care legislation was enacted in England. The 2014 Care Act included provisions pertaining directly to publicly financed social care, care-givers and continuity of care (UKGov 2014). The Act introduced national eligibility criteria for publicly financed and/or provided home care, including changes to care beneficiaries’ needs assessment processes and greater flexibility in the use of public financing for home care, allowing local authorities to publicly provide services, commission private home care services and/or provide direct payments to allow the recipient of home care to choose a provider themselves (UKGov 2014). However, the 2014 Care Act has been criticized for its vague language and broad criteria for eligibility assessment, and for requiring local authorities to take on greater responsibility without sufficient increases in financial and labour resources (Richards and Williamson Reference Richards and Williamson2015).
Importantly, much remains unknown about how effectively publicly financed care meets the needs of recipients. Prior studies often employ narrow definitions of unmet needs, typically referring to individuals who require home care support but receive no assistance – what can be termed ‘absolute unmet needs’ (Maplethorpe et al. Reference Maplethorpe, Darton and Wittenberg2014; Read et al. Reference Read, Hu, Dixon, Brimblecombe, Wittenberg, Brayne and Banerjee2022; Vlachantoni Reference Vlachantoni2019). This category of unmet needs, where no care is provided, forms the foundation of much of the existing literature, which predominantly consists of descriptive or cross-sectional studies (Desai et al. Reference Desai, Lentzner and Weeks2001; Murphy et al. Reference Murphy, Whelan and Normand2015; O’Brien et al. Reference O’Brien, Smuts, Fan, O’Sullivan and Warters2019; Read et al. Reference Read, Hu, Dixon, Brimblecombe, Wittenberg, Brayne and Banerjee2022). However, focusing solely on unmet needs overlooks situations where care is provided but is insufficient in fully meeting needs. Where this notion of partially met needs has been captured in the literature, such needs are frequently categorized under the broader umbrella of unmet needs, or referred to as ‘relative unmet needs’ (Calderón-Jaramillo and Zueras Reference Calderón-Jaramillo and Zueras2023; Potter Reference Potter2019; Schure et al. Reference Schure, Conte and Goins2015; Vlachantoni Reference Vlachantoni2019; Wilkinson-Meyers et al. Reference Wilkinson-Meyers, Brown, McLean and Kerse2014). This term describes instances where help is received but is not wholly adequate in meeting needs (Brimblecombe et al. Reference Brimblecombe, Pickard, King and Knapp2017; Iparraguirre Reference Iparraguirre2019). This study focuses on these more subjective perceptions of inadequacy in care delivery, but argues that these situations should instead be categorized as ‘under-met needs’ (Kennedy Reference Kennedy2001), as this term more accurately captures the nuances of care adequacy. It not only considers whether individual needs are addressed but also evaluates whether the provided services align with the recipient’s expectations.
Equally rare are studies examining the role of public financing in unmet need. Jenkins Morales and Robert (Reference Jenkins Morales and Robert2022) examined the relationship between types of long-term care services received by older Americans and unmet needs, finding that paid community care recipients had greater risk of reporting unmet need, as well as a greater risk of experiencing unmet need on an ongoing basis. However, there are few similar studies in the UK. Only one 2019 study examining social care services in the English context found reductions in community-based social care spending to be associated with higher odds of unmet long-term care needs (Iparraguirre Reference Iparraguirre2019). While this research explored the overall impact of broader funding cuts on the unmet needs of older people, there is still a lack of understanding of how public funding of home care services specifically impacts older people’s unmet or under-meet care needs. In addition, the study by Jenkins Morales and Robert (Reference Jenkins Morales and Robert2022) considered only absolute unmet need, with no specific focus on under-met need.
Thus, this study aims to explore how publicly financed care affects unmet and under-met needs among older adults. Specifically, it examines whether publicly financed care leads to a higher incidence of unmet or under-met needs compared to privately paid or informal care. This research offers new insights into the adequacy of care provision in the context of England’s social care system, particularly following the implementation of the Care Act 2014.
Conceptual framework
An adaptation of the Aday and Andersen (Reference Aday and Andersen1974) model of health-care utilization was developed to understand potential determinants of home care use; similar models have been previously employed in related literature (Murphy et al. Reference Murphy, Whelan and Normand2015). This model examines home care use as a function of predisposing factors, ‘the “propensity” of individuals to use services’; enabling factors, ‘the “means” individuals have available to them for the use of services’; and need factors, ‘illness level … perceived by the individual, or that evaluated by the delivery system’ (Aday and Andersen Reference Aday and Andersen1974, p. 213).
In the adapted model, the classification of home care services into publicly financed, privately paid and informal care acts as a critical enabling factor. This distinction is crucial for understanding access to and utilization of home care services. In this model, care adequacy is assessed through the lens of both unmet needs and under-met needs. Unmet needs refer to situations where individuals require care but receive no assistance, reflecting a complete absence of services despite the need for care (Read et al. Reference Read, Hu, Dixon, Brimblecombe, Wittenberg, Brayne and Banerjee2022; Vlachantoni Reference Vlachantoni2019). Meanwhile, under-met needs reflect situations where care is provided but is insufficient to meet the individual’s full range of care requirements (Brimblecombe et al. Reference Brimblecombe, Pickard, King and Knapp2017; Iparraguirre Reference Iparraguirre2019). This concept emphasizes not only the presence of care but also the degree to which that care aligns with the individual’s expectations and essential needs. By focusing on under-met needs, this study extends beyond traditional examinations of unmet needs and highlights the complexity of care provision in modern social care systems. Such a distinction better captures the nuances of how different funding sources directly affect the adequacy and accessibility of home care services. This is important, as existing reports from the Care Quality Commission (CQC) (2023) demonstrate that publicly financed care services often face significant resource constraints, impacting the quality and the quantity of care provided. These constraints may result in shorter visits, fewer care-givers and a higher likelihood of unmet or under-met needs. While these issues exist in private formal care, the CQC report outlines that this problem is more acute in local authority-funded care. Here, it is therefore hypothesized that individuals receiving publicly financed care are more likely to experience unmet and under-met needs compared to those receiving privately paid or informal care (Hypothesis 1).
Eligibility for publicly funded care is contingent upon meeting certain criteria, such as the level of need, availability of a carer and financial circumstances, as outlined in section 15(3) of the Care Act 2014. Furthermore, local authorities are mandated to review and potentially revise care and support plans if an individual’s circumstances change, which may lead to shifts between forms of care (Care Act 2014, s. 27). Approximately 55 per cent of publicly financed care recipients underwent care reviews in 2021–2022, with 19 per cent of reviews unplanned (NHS Digital 2022). While no specific metrics are readily available as to movement between types of care, regular reassessment of needs, alongside tight budgets and growing demand, suggest that shifts in eligibility may not be uncommon, with some no longer receiving publicly financed care.
Regarding the quality of different types of home care, informal care-givers, typically family members or close friends, though often untrained in caring, can theoretically provide highly personalized care tailored to the recipient’s needs and preferences (Kim et al. Reference Kim, Wister, O’dea, Mitchell, Li and Kadowaki2023). Privately paid formal care may provide faster access to care, with 53 per cent of recipients reporting that private care enabled them to be seen more quickly (Care Quality Commission 2023). Informal care, either alone or in combination with formal care, has been shown to improve health outcomes (Coe et al. Reference Coe, Konetzka, Berkowitz, Blecker and Van Houtven2021). This evidence suggests that transitions to privately paid or informal care may offer greater flexibility in addressing unmet needs and under-met needs, particularly when public care services are constrained.
Therefore, it is hypothesized that individuals transitioning from publicly financed care to privately paid or informal care may experience a reduction in unmet needs and under-met needs over time (Hypothesis 2). Nevertheless, this outcome is contingent on factors such as the individual’s care needs, the availability of informal support and the affordability of private care.
Methods
Data and sample
This study draws upon nationally representative survey data from the English Longitudinal Study of Ageing (ELSA). Details on data collection, including the sampling strategy, consent processes and protocols, can be found within the study documentation (Banks et al. Reference Banks, Batty, Breedvelt, Coughlin, Crawford, Marmot, Nazroo, Oldfield, Steel, Steptoe, Wood and Zaninotto2023). The sample includes community-dwelling adults over 50 years old. The sample is restricted to those present in waves 6–9 (2013–2019), as changes in the format and wording of key questions relating to home care support limit the ability to compare waves 6–9 with earlier waves of the survey.
The original survey included 10,601 participants in wave 6, which decreased to 8,736 in wave 9 owing to attrition. This study focuses on individuals aged 50 and over who reported difficulties with one or more activities of daily living (ADLs) or instrumental activities of daily living (IADLs). The sample includes individuals who met these criteria and participated in all four waves, and reported using home care services, forming the final analytical sample of 340 participants (1,360 observations) (Figure 1).

Figure 1. Sample selection flowchart.
Notes: ADL: activity of daily living; IADL: instrumental activity of daily living.
Source: Author’s construction using ELSA wave 6 to wave 9.
Dependent variables
In this study, unmet need for home care services is operationalised as self-reported difficulties with at least one ADL (eating, bathing, dressing, toileting, transferring, ambulating) or IADL (shopping, managing medication, preparing meals, paying bills, doing housework) as well as the respondent self-reporting that they received no help with that task (see Figure 2). Specifically, the number of ADLs and IADLs for which the respondent reported difficulty but also for which they reported receiving no help is examined. The ELSA survey includes questions that identify whether the respondent has difficulties with specific ADLs and IADLs, as well as whether or not they received assistance with performing each ADL or IADL.

Figure 2. Operationalizing unmet need and under-met need for social care.
In ELSA, where assistance with ADL(s) and IADL(s) is received, respondents are asked an overall question about whether that assistance ‘always’, ‘usually’, ‘sometimes’ or ‘hardly ever’ meets their needs. The term ‘under-met need’ is used here to refer to instances in which respondents reported receiving help with ADL and/or IADL limitations, but indicated that the help received did not always meet their needs. Therefore, responses of ‘usually’, ‘sometimes’ or ‘hardly ever’ are included in the operationalization of under-met need (see Figure 1), similar to previous research (Peng et al. Reference Peng, Wu and Ling2015). Because of the way under-met need is captured in ELSA, it is a binary variable in these models.
Sensitivity analyses were performed exploring alternate operationalizations of under-met need, where we included only those responses of ‘sometimes’ and ‘hardly ever’, or simply ‘hardly ever’, in the operationalization of under-met need. However, primarily owing to the small sample sizes in ELSA (for example, only 79 individuals selected responses of ‘sometimes’ and ‘hardly ever’), these models failed to converge. It also suggests either that such under-met needs are relatively rare within the population we studied or that there are potential floor effects impacting responses.
Independent variables
Within the modified Aday and Andersen (Reference Aday and Andersen1974) conceptual framework, predisposing factors are operationalized as gender, age, marital status and number of household members. Scholars have found that lower household wealth and house ownership (having a mortgage versus full house ownership) are associated with higher levels of unmet need (Cao et al. Reference Cao, Feng, Mor and Du2023; Dunatchik et al. Reference Dunatchik, Icardi, Roberts and Blake2016; Wilkinson-Meyers et al. Reference Wilkinson-Meyers, Brown, McLean and Kerse2014). Thus, enabling factors include total household net non-housing wealth, employment status and household ownership. Need factors include cognitive status, whether the respondent has one or more chronic disease and the number of reported ADL and/or IADL limitations. Self-reported health status is not included primarily because research has shown that self-reported health status is often influenced by factors already captured by our models, such as the presence of chronic conditions and functional limitations (Banerjee et al. Reference Banerjee, Perry, Tran and Arafat2010; Whitmore et al. Reference Whitmore, Markle-Reid, Fisher, McAiney and Ploeg2021, Reference Whitmore, Markle-Reid, McAiney, Ploeg, Griffith, Phillips, Wister and Fisher2022). Thus, the inclusion of self-reported health status can lead to covariance problems in regression models.
Cognitive status
This project draws upon the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE), a subjective proxy report of changes in behaviour and cognition (Cadar et a., Reference Cadar, Lassale, Davies, Llewellyn, Batty and Steptoe2018; Jorm Reference Jorm2004; Read et al. Reference Read, Hu, Dixon, Brimblecombe, Wittenberg, Brayne and Banerjee2022). The IQCODE ranges from 1, indicating improving proxy-reported subjective cognitive function, to 5, indicating significantly worsening cognitive function. Descriptive analyses differentiate between those with IQCODE scores above and below 3.38, as this threshold has previously been used in the literature as indicating probable dementia (Cader et al, Reference Cadar, Lassale, Davies, Llewellyn, Batty and Steptoe2018; Quinn et al. Reference Quinn, Fearon, Noel-Storr, Young, McShane and Stott2014).
Types of home care
In ELSA, respondents who report receipt of assistance with ADL(s) and IADL(s) are asked to specify the type of care received for each difficulty. While this level of detail is valuable, it introduces complexity because respondents may rely on multiple types of service for different difficulties. Consequently, differentiating between distinct types of service use requires careful consideration.
In this study, home care was considered to be publicly financed if the respondent reported that their local authority/council/social services (a) manages home care payments for them, (b) allocates money for home care services via direct payment and/or (c) provides a home care worker/nurse, health visitor or district nurse/member of staff to assist them. This is compared to other sources, including informally provided care (unpaid care provided by family or friends) and formal care that was paid for privately.
To strategically address the complexity in differentiating between distinct types of service use, two approaches to categorizing care type were developed through an exploration of methods of categorization used in the wider literature (e.g. Lau et al. Reference Lau, Leeb, English, Graham, Briggs, Brody and Marshall2005; Petrenko et al. Reference Petrenko, Friend, Garrido, Taussig and Culhane2012): a hierarchical approach and a predominant type approach. The main analyses for this study use the former approach where care type is based on a hierarchy: that is, if participants receive publicly financed care, they are classified under publicly financed care, regardless of any additional care types they might use. If they do not receive publicly financed care but use privately paid formal care, they are classified under privately paid care. Remaining care recipients are classified as receiving only informal care. This hierarchical approach enables an examination of the effects of care type in a structured way, assessing impact on unmet and under-met needs when publicly financed care is present versus absent, and how additional types contribute when public funding is unavailable.
In the predominant type approach, each participant was assigned to the care type they use the most often. For example, if someone uses informal care most frequently, they are categorized as an informal care user, even if they also receive publicly financed or privately purchased services. However, this method does not isolate the impact of each type and, as ELSA does not quantify the amount of care received (e.g. in hours/week), it is arguably difficult to robustly capture predominance. Sensitivity analyses were performed using this approach, which are available in the supplementary materials for comparison.
Analysis
Descriptive statistics are presented to illustrate sample characteristics at baseline (wave 6) and to illustrate the distribution of unmet and under-met need by key sample characteristics across the study period (waves 6–9). Two types of analytical models are used: longitudinal fixed effects and pooled cross-sectional regression models. To examine changes in the number of unmet needs over time and factors influencing the number of unmet needs, longitudinal fixed effects Poisson models and pooled cross-sectional Poisson models (Wooldridge Reference Wooldridge2010) are used, respectively. Poisson models provide more consistent and robust estimators in short panel settings (Wooldridge Reference Wooldridge1999), and allow for fixed effects estimation. Although negative binomial models are commonly used for over-dispersed count data, they are less well-suited to fixed effects longitudinal panel analysis (Guimaraes Reference Guimaraes2008; Hilbe Reference Hilbe2014). Therefore, Poisson models with robust standard errors to correct for over-dispersion were employed as they offer a more appropriate approach for panel data structures with individual fixed effects. The use of robust standard errors to minimize the problem of correlated error terms in our pooled models and over-dispersion of our key variables follows prior literature (Andreß et al. Reference Andreß, Golsch and Schmidt2013; Wooldridge Reference Wooldridge1999). To examine changes in under-met need over time and factors associated with under-met need, longitudinal fixed-effects and pooled cross-sectional logistic regression models were used, respectively. By employing both longitudinal fixed effects and pooled cross-sectional regression models, this study leverages the strengths of each to provide a more comprehensive understanding of the impact of home care services on older people’s unmet and under-met needs.
As the official longitudinal weights provided by ELSA are based on samples of wave 1 or wave 4 data, we constructed our own longitudinal weights using the official ELSA cross-sectional weights for wave 6 data and multiplied these by the reverse probability weighting coefficients between each wave (Andreß et al. Reference Andreß, Golsch and Schmidt2013). Reverse probability weighting coefficients were derived from a logit regression of whether the respondent had participated in the previous wave (Andreß et al. Reference Andreß, Golsch and Schmidt2013). These constructed longitudinal weights were used in all analyses. Analyses were conducted in Stata version 15.
Results
Table 1 presents weighted and unweighted descriptive statistics for the baseline sample (wave 6). In the weighted sample, most (77.13 per cent) relied on informal care alone, while 15.61 per cent used privately paid care (which may include both private paid and informal care, or private paid care alone), and 7.26 per cent received publicly financed care (which may include combinations such as publicly financed care alone, publicly financed and private paid care, publicly financed and informal care, or all three types). This underlines the role of informal care and the relative rarity of publicly financed care (alone or in combination). The sample had a weighted mean age of 66.4 at baseline and 68.35 per cent were female. The weighted mean baseline IQCODE score was 0.02 (SD 0.3), suggesting that most had not experienced worsening cognition. The baseline weighted mean number of ADL and IADL limitations was 3.9 (SD 2.4). The baseline weighted mean number of unmet needs was 6.9 (SD 2.2) and approximately 42.84 per cent of our sample reported under-met needs.
Table 1. Sample characteristics at wave 6, 2012–2013

Source: Author constructed based on ELSA wave 6.
Notes: 1 Under-met need is defined as a respondent reporting difficulties with one or more activities of daily living (ADLs) or instrumental activities of daily living (IADLs) and reporting that they receive help with that/those ADL(s) or IADL(s), but that the help they receive does not always meet their needs.
2 The sample includes core ELSA members, aged 50+, interviewed in all four ELSA waves 6–9. The sample excludes those with no ADL or IADL difficulties and who receive no home care.
3 Employment status is operationalized as retired or other employment status; the latter includes those who are employed and as well as those inactive in the labour market.
4 Respondent reported having one or more chronic condition or disease.
5 Care was considered to be publicly financed if the respondent reported that: (a) their local authority/council/social services manages social care payments for them, (b) their local authority/council/social services allocates money for social care services via a direct payment and/or (c) help they received with ADLs or IADLs came from a local authority or social services helper.
6 Total number of ADLs or IADLs with which the respondent reported having difficulty and for which they reported receiving no help.
7 The number of observations varies because of missing values on some variables.
8 Informant Questionnaire on Cognitive Decline in the Elderly score.
9 Total number of ADL and IADL limitations.
10 The number of household members ranges from 1 to 6.
The unadjusted distribution of unmet and under-met need by participant characteristics and year is presented in Table 2. Those receiving publicly financed care had a lower weighted mean number of unmet needs over time compared to those receiving privately paid or informal care. However, the weighted proportion of under-met needs was highest among those receiving publicly financed care, particularly in 2019, where 66.5 per cent reported under-met needs compared to 40.4 per cent of those using privately paid care and 35.5 per cent of those relying exclusively on informal care.
Table 2. Distribution of unmet and under-met needs based on characteristic variables, 2013–2019 (weighted)
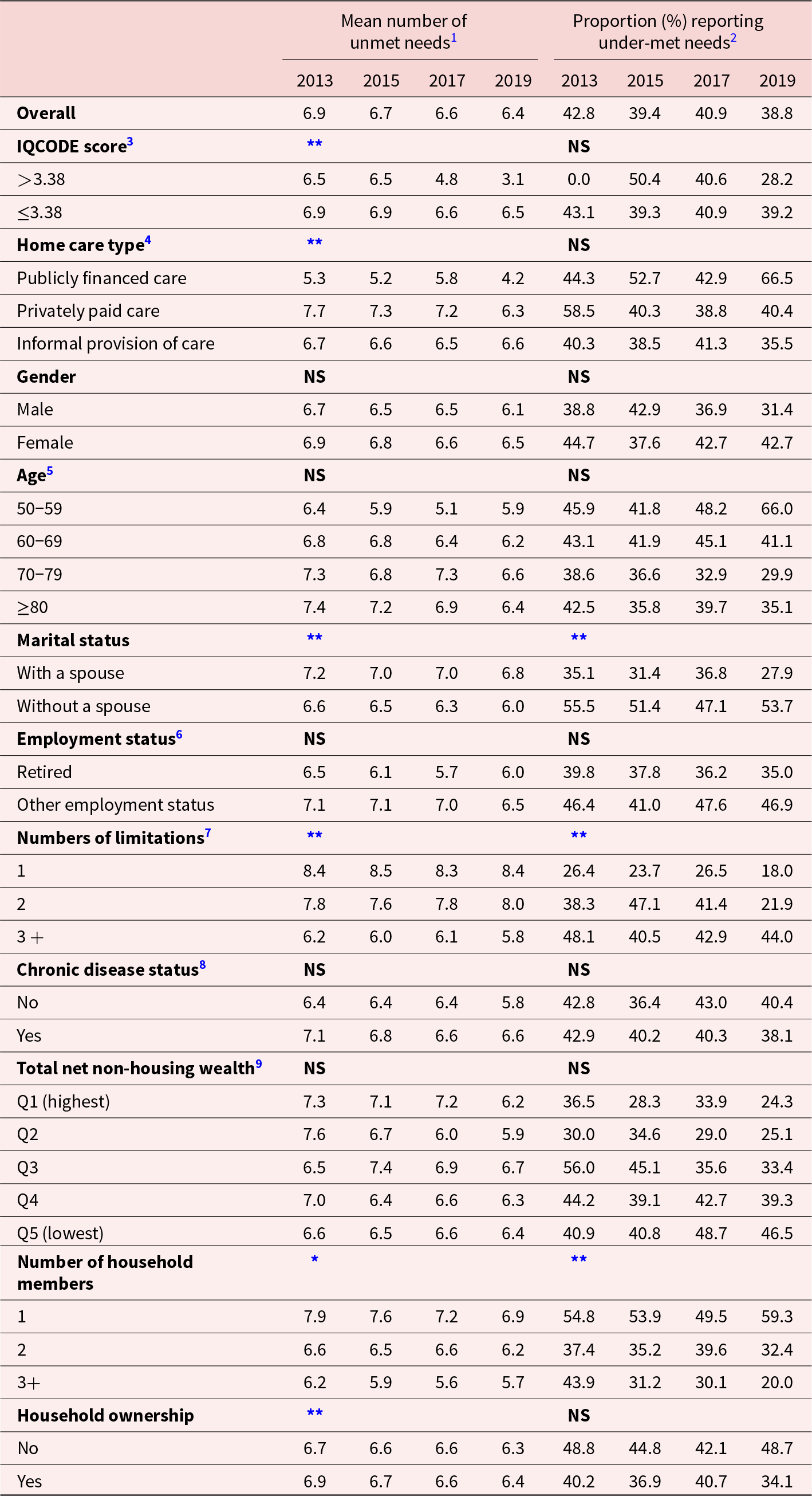
Source: Author constructed based on ELSA waves 6–9.
* Notes: Significance level: p < 0.05, ** p < 0.01. NS: not statistically significant.
1 Mean number of ADLs or IADLs with which the respondent reported having difficulty and for which they reported receiving no help (range: 0–11).
2 Under-met need is defined as a respondent reporting difficulties with one or more activities of daily living (ADLs) or instrumental activities of daily living (IADLs) and reporting that they receive help with that/those ADL(s) or IADL(s), but that the help they receive does not always meet their needs.
3 Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) score is shown as a binary variable for ease of interpretation. Previous empirical research considers respondents scoring above a threshold of 3.38 as indicating probable dementia (Cadar et al. Reference Cadar, Lassale, Davies, Llewellyn, Batty and Steptoe2018; Quinn et al. Reference Quinn, Fearon, Noel-Storr, Young, McShane and Stott2014). Subsequent models treat IQCODE as continuous.
4 Care was considered to be publicly financed if the respondent reported that: (a) their local authority/council/social services manages social care payments for them, (b) their local authority/council/social services allocates money for social care services via a direct payment and/or (c) help they received with ADLs or IADLs came from a local authority or social services helper.
5 Age is shown as a categorical variable for ease of interpretation. Subsequent models treat age as continuous.
6 Employment status is operationalized as retired or other employment status (employed or inactive in the labour market).
7 Total number of ADL and IADL limitations.
8 Respondent reported one or more chronic condition or disease.
9 Wealth quintiles, with Q1 denoting highest wealth and Q5 denoting lowest wealth. Subsequent models treat wealth as continuous.
The weighted mean number of unmet needs reported by all respondents (n = 340) decreased from 6.9 in wave 6 (2013) to 6.4 in wave 9 (2019). The weighted proportion reporting under-met needs decreased from 42.8 per cent in wave 6 to 38.8 per cent in wave 9. Among those with IQCODE scores above 3.38 (indicating probable dementia), the mean number of unmet needs decreased from 6.5 in wave 6 to 3.1 in wave 9. While none of those with IQCODE scores above 3.38 reported under-met need in waves 6, under-met need in this group jumped to 40.6 per cent in wave 8, then fell to 28.2 per cent in wave 9. Those with three or more ADL or IADL limitations reported a slight reduction in the mean number of unmet needs, and an initial decrease followed by a slight increase in under-met needs across the study period.
Table 3 presents the results of the analytical models examining the factors associated with the number of unmet needs, with a particular focus on care type. Longitudinal fixed effects Poisson results (columns 2–3) show no statistically significant association between changes in the type of home care received (e.g. transitioning from publicly financed to other types of care) and number of unmet needs. However, the pooled cross-sectional analyses (columns 4–5) find that informal care is significantly associated with a higher incidence of unmet needs compared to receiving publicly financed care (incidence rate ratio (IRR) 1.16; 95% confidence interval (CI) 1.06–1.27, p < 0.01), as is receiving privately paid care (IRR 1.17; 95% CI 1.07–1.28, p < 0.01). Publicly financed care may therefore provide an advantage in reducing unmet needs, even when delivered in combination with informal and/or private care.
Table 3. Number of unmet needs and changes in the number of unmet needs for ADL and IADL support, 2013–2019

Source: Author constructed based on ELSA waves 6–9.
*** Notes: Significance level: p < 0.001, ** p < 0.01, * p < 0.05.
1 A longitudinal Poisson fixed effects model examining factors associated with changes in the number of unmet needs.
2 A pooled Poisson model examining factors associated with number of unmet needs.
3 IRR: incidence rate ratio.
4 Informant Questionnaire on Cognitive Decline in the Elderly score.
5 Care was considered to be publicly financed if the respondent reported that: (a) their local authority/council/social services manages social care payments for them, (b) their local authority/council/social services allocates money for social care services via a direct payment and/or (c) help they received with ADLs or IADLs came from a local authority or social services helper.
6 Gender was excluded from the fixed effects model because it is time invariant.
7 As the effect of age may be non-linear, the square of age was included to model the effect of age more appropriately.
8 Employment status is operationalized as retired or other employment status (employed or inactive in the labour market).
9 Total number of ADL and IADL limitations.
10 Respondent reported one or more chronic condition or disease.
11 To capture the potential impact of the 2014 Care Act, year dummy variables were included. The reference year is 2017 (wave 8) because ELSA wave 7 data collection partially covered the period before enactment, 2014–2015, and because we hypothesized a lagged impact of the policy.
Looking at factors beyond care type, the longitudinal fixed effects Poisson results (columns 2–3) find that an increasing IQCODE score, indicating worsening cognition, is associated with a lower incidence rate of unmet need, with a one-point increase in the IQCODE score associated with a 5 per cent decrease in the incidence rate of unmet need over time (IRR 0.95; 95% CI 0.91–0.98, p < 0.01). Each additional ADL and IADL limitation is associated with a 7 per cent decrease in the incidence rate of unmet need over time (IRR 0.93; 95% CI 0.92–0.93, p < 0.001). Household ownership, a proxy for higher socio-economic status, is associated with an increase in the incidence rate of unmet need (IRR 1.29; 95% CI 1.07–1.54, p < 0.01). Year was also statistically significant, with a 19 per cent decreased incidence rate of unmet need in 2013 versus 2017 (IRR 0.81; 95% CI 0.66–0.99, p < 0.05) and an 11 per cent decreased incidence rate of unmet needs in 2015 versus 2017 (IRR 0.89; 95% CI 0.80–0.98, p < 0.05).
Pooled cross-sectional analyses (columns 4–5 of Table 3) demonstrate similar patterns. A higher IQCODE score, indicating worsening proxy reported cognitive status, is associated with lower incidence of unmet needs (IRR 0.93; 0.89–0.98, p < 0.01). Having more ADL and IADL limitations (IRR 0.91; 95% CI 0.90–0.92, p < 0.001) and more household members (IRR 0.96; 95% CI 0.92–0.99, p < 0.05) are also associated with lower incidence of unmet needs.
Table 4 presents the results of our analyses examining under-met need. Longitudinal fixed-effects model results (columns 2–3) indicate that transitioning from publicly financed to informal care significantly reduces the odds of under-met need (odds ratio (OR) 0.48; 95% CI 0.23–0.56). In contrast, transitions from publicly financed to privately paid care do not statistically significantly impact under-met needs (OR 0.53; 95% CI 0.25–1.13). The pooled cross-sectional model (columns 4–5) shows that neither privately paid (OR 0.95; 95% CI 0.61–1.48) nor informal care (OR 0.80; 95% CI 0.54–1.21) is significantly associated with under-met needs.
Table 4. Odds of under-met need and changes in the odds of under-met need, 2013–2019
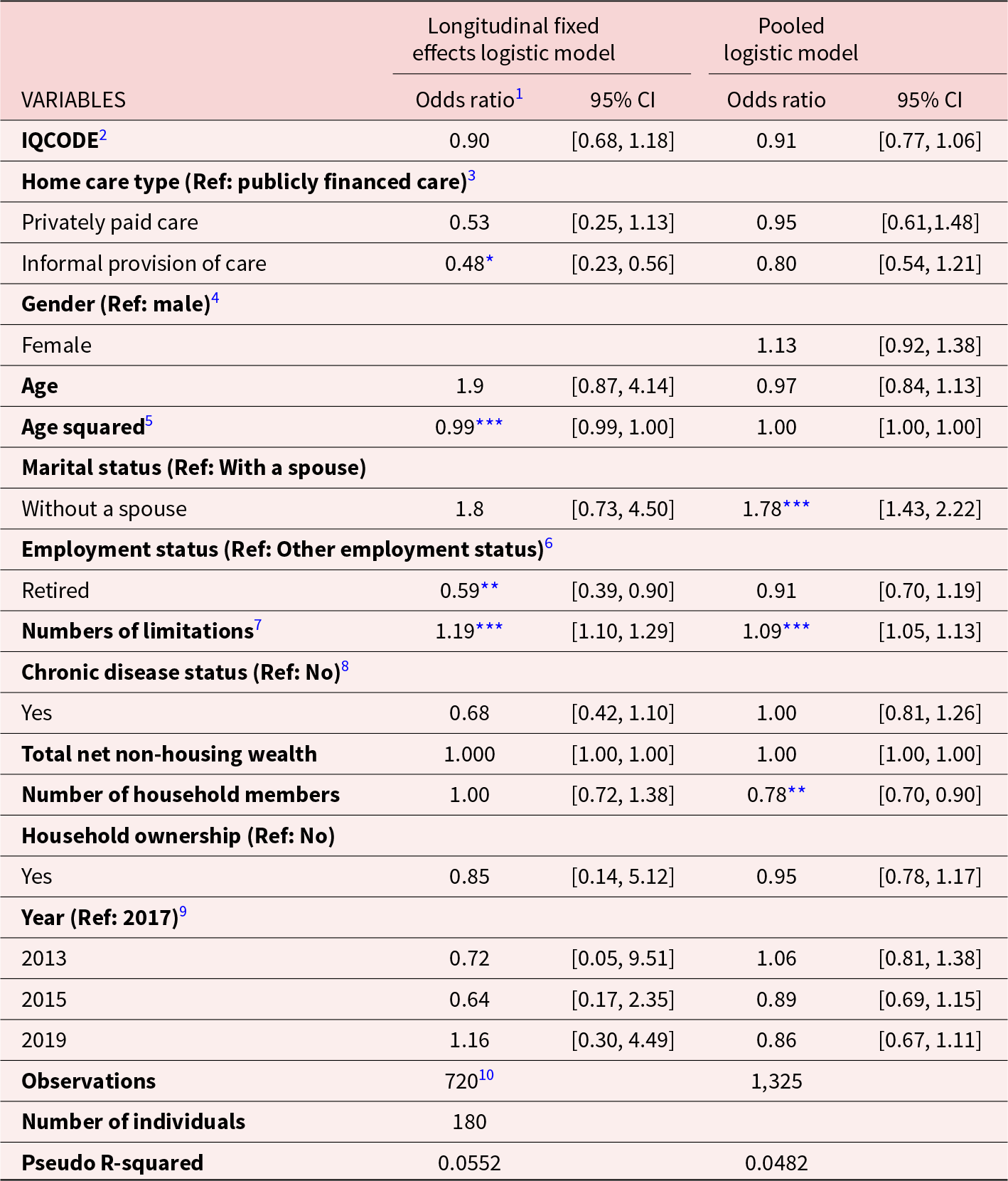
Source: Author constructed based on ELSA waves 6–9.
*** Notes: Significance level: p < 0.001, ** p < 0.01, * p < 0.05.
1 Odds ratio (OR) = 1 indicates that the independent variable has no effect on under-met need; OR > 1 indicates increased odds of under-met need; OR < 1 indicates decreased odds of under-met need.
2 Informant Questionnaire on Cognitive Decline in the Elderly score.
3 Care was considered to be publicly financed if the respondent reported that: (a) their local authority/council/social services manage social care payments for them, (b) their local authority/council/social services allocates money for social care services via a direct payment and/or (c) help they received with ADLs or IADLs came from a local authority or social services helper.
4 Gender was excluded from the fixed effects model because it is time invariant in the data.
5 As the effect of age may be non-linear, the square of age was included to model the effect of age more appropriately.
6 Employment status is operationalized as retired or other employment status (employed or inactive in the labour market).
7 Total number of ADL and IADL limitations.
8 Respondent reported one or more chronic condition or disease.
9 To capture the potential impact of the 2014 Care Act, year dummy variables were included. The reference year is 2017 (corresponding to wave 8) rather than 2015 because ELSA wave 7 data collection covered some of the period just before enactment, 2014–015, and because we hypothesized a lagged impact of the policy.
10 We excluded 640 observations owing to no variation over time.
Longitudinal fixed effects analyses find that the number of ADL or IADL limitations is significantly associated with increased odds of under-met needs, with one additional limitation associated with 19 per cent increased odds of under-met need over time (OR 1.19; 95% CI 1.10–1.29, p < 0.001). Transitioning from being employed or inactive in the labour market to being retired is associated with 41 per cent reduced odds of experiencing under-met need (OR 0.59; 95% CI 0.39–0.90, p < 0.01).
Pooled cross-sectional models find each additional ADL or IADL limitation to be associated with 9 per cent greater odds of reporting that needs are under-met (OR 1.09; 95% CI 1.05–1.13, p < 0.001). Not having a spouse is associated with 78 per cent greater odds of under-met need (OR 1.78; 95% CI 1.43−2.22, p < 0.001). Each additional household member is associated with 22 per cent lower odds of under-met need (OR 0.78; 95% CI 0.70−0.90, p < 0.01).
Discussion
This study provides insights into the factors influencing unmet and under-met needs for home care among adults aged over 50 in England. A significant contribution of this study lies in its comparison of publicly financed, privately paid and informal care, adding to the literature on care adequacy.
Types of home care and unmet needs
The findings are consistent with extant literature on unmet needs, including studies by Vlachantoni (Reference Vlachantoni2019) and Vlachantoni et al. (Reference Vlachantoni, Evandrou, Falkingham and Qin2024), which highlight the persistent issue of unmet social care needs among older individuals in England. Vlachantoni et al. (Reference Vlachantoni, Evandrou, Falkingham and Qin2024) emphasize the dynamic nature of need, demonstrating that unmet needs are often experienced repeatedly by those with declining health or limited social support. We expand on these findings by differentiating between types of home care, revealing that public funding is associated with lower levels of unmet need, suggesting the existence of care gaps for individuals relying primarily on privately paid or informal care. Similar to findings by Calderón-Jaramillo and Zueras (Reference Calderón-Jaramillo and Zueras2023), these results also suggest that while informal care remains a prevalent and valuable resource, it may not comprehensively address all care needs. Calderón-Jaramillo and Zueras (Reference Calderón-Jaramillo and Zueras2023) further highlight that Mediterranean countries with family-centred systems reliant on informal care experience higher levels of unmet needs compared to more welfare state-oriented systems such as in Nordic countries. This is in line with our finding that publicly financed care may play a stabilizing role, effectively reducing the number of unmet needs.
However, the findings from this study contrast with literature suggesting that private care might reduce unmet needs (e.g. Freedman and Spillman Reference Freedman and Spillman2014). This discrepancy may reflect differences in the scope and delivery of publicly financed care across settings (England versus the United States), as well as variations in the types of support prioritized through different care arrangements. These differences underscore the need to examine specific service structures within public funding models to identify which types of care most effectively reduce unmet needs.
Results also suggest that informal care alone may be insufficient in fully meeting needs, particularly for those with higher levels of dependency. This finding is consistent with studies such as Miranda-Castillo et al. (Reference Miranda-Castillo, Woods and Orrell2010) and from Age UK (Reference Age2014), which find that informal care provision often lacks the resources and structure necessary to meet the needs of adults with severe limitations. Our study thus reinforces the notion that informal care may differ from formal, publicly financed services in ways that need to be better understood, particularly for those with complex, multi-faceted needs.
Types of home care and under-met needs
While we initially hypothesized that transitions from publicly financed care to either informal or privately financed care would increase under-met needs, the results showed a more complex pattern. In the longitudinal fixed-effects model, moving from publicly financed care to informal care was associated with a significant reduction in under-met needs. This may reflect that informal care, as a primary source of support, can provide more personalized attention that better meets specific needs (Kim et al. Reference Kim, Wister, O’dea, Mitchell, Li and Kadowaki2023), especially as individuals move away from formal, structured support.
However, in the pooled cross-sectional model, neither privately paid nor informal care showed a significant association with under-met needs when compared to publicly financed care. This discrepancy may highlight the limitations of cross-sectional analysis in capturing the dynamic and personalized nature of informal care over time. These differences also highlight the importance of contextual and temporal factors in care provision, as also noted by Vlachantoni et al. (Reference Vlachantoni, Evandrou, Falkingham and Qin2024), who discuss how social and familial contexts influence unmet need dynamics across time. Our results imply that there is a critical distinction between access to care and the adequacy of that care. While receiving publicly financed care is associated with a reduction in unmet needs, it does not always equate to fully meeting all care needs, often resulting in under-met needs.
Other key findings: vulnerability and access to support
Findings reveal that individuals with worsening cognitive function and more ADL and IADL limitations tend to report fewer unmet needs for ADL/IADL support, in line with the finding of a similar study by Jenkins Morales and Robert (Reference Jenkins Morales and Robert2022) in the United States. Symptom progression over time, such as worsening cognition and increasing ADL/IADL limitations, was associated with a decrease in unmet needs. This suggests that greater vulnerability may trigger access to home care support services.
These results highlight the complexity of care needs among older adults. While more vulnerable individuals appear to receive targeted support, the care they receive may still be insufficient, pointing to gaps in adequately meeting the needs of those with more complex conditions. The interplay between vulnerability and access to services presents an area for further research, particularly in understanding the quality of care provided to individuals with increasing needs.
Implications for policy and practice
In 2015, in the middle of our study period, the 2014 Care Act was implemented. It signalled a major policy shift aimed at reforming home care financing and delivery in England. A key sub-aim of this study was to assess the impact of this policy on the prevalence and severity of unmet and under-meet needs among adults aged over 50. Consistent with the concerns raised by Richards and Williamson (Reference Richards and Williamson2015) regarding the Act’s vague mandates and the burden on local authorities, the findings suggest that there is little evidence of impact of this policy change over the study period. In fact, a statistically significant increase in the rate of unmet needs in 2017 versus 2013 may, if anything, suggest a lagged negative effect of the Care Act, though there is insufficient evidence for this to be a conclusive finding. This aligns with broader international experiences, such as in Australia, where policy shifts have struggled to immediately translate into improved care outcomes (Calder et al. Reference Calder, Dunkin, Rochford and Nichols2019). Future research should investigate the effect of the Care Act in greater depth, more closely examining the multiple pathways through which this major national legislation may have had an impact at both the local authority and the individual levels.
More broadly, this study raises some important questions around the ways in which adults with care needs are (or are not) supported to live at home. As population ageing accelerates, it will become increasingly crucial for policy makers to consider difficult questions around priority setting between home care and wider public health priorities, as well as how best to allocate resources within home care. In England, as in most nations, current public financing levels are inadequate to meet the support needs of all adults with care needs living at home, and this study suggests that important trade-offs are being made – whether implicit or explicit – in the allocation of resources to and within home care. Further, more nuanced investigations into unmet and under-met need will help provide crucial evidence to support future home care policy making.
Limitations
Notwithstanding the original contributions of the analyses presented here, there are important limitations to this work. One limitation is that the assessment of unmet and under-met need centres on ADL and IADL difficulties. This is owing in part to available data, but also reflects contemporary home care policies (UKGov 2014). Specifically, ADLs and IADLs are integral to needs assessments as they capture essential functional limitations that typically trigger formal care services, particularly within publicly funded systems (Freedman and Spillman Reference Freedman and Spillman2014). Moreover, eligibility for home care services often hinges on these metrics, with thresholds for support being set based on individuals’ (in)ability to perform these tasks independently.
However, despite the centrality of ADLs and IADLs in determining access to care in the English system – as well as in other countries with similar home care structures – these measures offer a relatively narrow view of need. Critics argue that this focus can overlook other significant aspects of wellbeing and quality of life, such as emotional support and social engagement, which are often just as important to care recipients (Richards and Williamson Reference Richards and Williamson2015). By concentrating on functional limitations, there is a risk of excluding broader personal outcomes that older adults themselves may prioritize, such as maintaining independence or achieving personal goals within their daily lives.
The exploration of under-met need addresses this concern to some extent, as the concept of under-met need seeks to move beyond the binary determination of whether support is provided, to capture whether the care provided aligns with the recipient’s expectations and personal goals. Future work might explore a wider range of definitions of unmet need for home care support, incorporating care recipients and care-giver perspectives.
Another limitation relates to the hierarchical approach, which, while useful for isolating the impact of care types, has limitations. It simplifies mixed care arrangements by assigning each individual to a single primary category, potentially underestimating the cumulative effects of mixed care or overemphasizing the impact of publicly financed care. Consequently, the hierarchical approach may not fully capture the nuanced reality of multi-faceted care arrangements.
Another limitation is the reliance on self-reports or proxy reports to assess unmet and under-met care needs, which introduces potential sources of bias. Proxy responses in particular may not fully reflect care recipients’ experiences or perceptions. Additionally, social desirability bias may lead to more positive reporting on the care received, which could explain the low selection of intermediate response options of ‘sometimes’ and ‘hardly ever’ (Krosnick et al. Reference Krosnick, Holbrook, Berent, Carson, Hanemann, Kopp, Mitchell, Presser, Ruud, Smith, Moody, Green and Conaway2002; Stocke Reference Stocke2007).
Furthermore, the small number of individuals (n = 27) receiving publicly financed care limits the robustness and generalizability of conclusions specific to this care type. Although sampling weights were used to address selection biases, the limited sample size for publicly financed care necessitates a conservative interpretation of results. Future research using larger samples and direct self-reports, when possible, would validate and strengthen the findings regarding unmet and under-met needs.
Finally, while the ELSA dataset is a nationally representative sample of UK adults aged 50+, providing a solid basis for analysing ADL and IADL limitations, the ethnic diversity of this sample is limited. The ELSA data primarily categorize individuals into ‘White’ and ‘Non-White’ groups, which does not provide a comprehensive picture of the ethnic diversity of the UK population. This broad categorization limits the ability to explore whether patterns of unmet and under-met needs differ across more specific groups. Future research should aim to incorporate more detailed breakdowns by ethnicity to better understand differences in unmet and under-met needs across communities.
Conclusion
This study has comprehensively analysed the impact of public financing on unmet and under-met home care needs among English adults aged over 50, utilizing data from the English Longitudinal Study of Ageing (ELSA) waves 6 to 9. The findings reveal that while individuals with more ADL and IADL limitations, or worsening cognition, generally receive home care support, this support often does not fully meet their needs. This underscores a persistent care deficit despite policy efforts aimed at improving care accessibility and effectiveness.
This study sought to illuminate the differential impacts of publicly funded versus other types of home care, particularly in light of the 2014 Care Act’s implementation. Unlike previous studies that have predominantly focused on the presence of unmet needs, this research provides a nuanced perspective by also considering the adequacy of the care received. By evaluating both unmet and under-met needs, this study contributes a more granular understanding of the care dynamics under different financing schemes.
In addition, this study makes a notable methodological contribution by adapting the Aday and Andersen (Reference Aday and Andersen1974) model of health-care utilization for a novel purpose. This modification enhances its applicability to contemporary home care scenarios, providing a more accurate framework for assessing the impact of different care types on unmet and under-met needs. This refined model can serve as a valuable tool for researchers exploring similar issues in various health-care systems globally.
While situated within England, these results resonate with broader comparative research, such as Calderón-Jaramillo and Zueras (Reference Calderón-Jaramillo and Zueras2023), which reveals similar care challenges across different social care systems in Europe. Cross-country comparisons could provide deeper insights into how different funding mechanisms affect care quality and satisfaction among older people.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0144686X25100160.
Author contributions
They were as follows: FW: conceptualization, data curation, formal analysis, writing – original draft, writing – review and editing; KT: conceptualization, supervision, writing – review and editing; ST: conceptualization, supervision, writing – review and editing; RL: writing – original draft; EA: conceptualization, supervision, writing – original draft, writing – review and editing, funding acquisition. We are grateful for the contributions of Sofia de la Fuente Garcia, PhD who was involved in initial project meetings, but did not meet the criteria for authorship of this manuscript. This manuscript was improved by feedback from Professor Athina Vlachantoni and Dr Krista L. Harrison.
Financial support
This work was supported by the Global Brain Health Institute (GBHI), the Alzheimer’s Association and the Alzheimer’s Society [GBHI ALZ UK-21-721057].
Competing interests
The authors declare no competing interests.
Ethical standards
This study received ethical approval from the University of Edinburgh (reference number 279119).








