Impact statement
This study highlights the role of resilience in determining the mental health outcomes of young Kenyans who have experienced adverse childhood experiences (ACEs). Resilience mediates and moderates the effects of ACEs on depression, post-traumatic stress disorder (PTSD), and suicidality. This calls for policies and initiatives that strengthen resilience in our study community population. Despite being a powerful protective factor against depression and PTSD, the impact of resilience on suicidality differs according to the kind of ACE, which emphasizes the necessity for targeted intervention.
Introduction
Adverse childhood experiences (ACEs) consists of a spectrum of traumatic events occurring before the age of 18 years and include various forms of abuse, neglect, and household dysfunction (Youssef et al., Reference Youssef, Green, Dedert, Hertzberg, Calhoun, Dennis and Beckham2013; Schulz et al., Reference Schulz, Becker, Van der Auwera, Barnow, Appel, Mahler, Schmidt, John, Freyberger and Grabe2014). ACEs are becoming more widely acknowledged as a serious public health issue with profound effects on mental health and overall well-being (Sasidharan and Talwar, Reference Sasidharan and Talwar2023; White et al., Reference White, Prasad, Ammar, Yaun and Shaban-Nejad2024), and in particular resulting in depression, post-traumatic stress disorder (PTSD), and suicidality (Benarous et al., Reference Benarous, Raffin, Bodeau, Dhossche, Cohen and Consoli2017; Burstein and Greenfield, Reference Burstein and Greenfield2020; Ashaba et al., Reference Ashaba, Cooper-Vince, Maling, Satinsky, Baguma, Akena, Nansera, Bajunirwe and Tsai2021). The World Health Organization highlights ACEs as a critical public health issue and calls for continued efforts to develop interventions to reduce ACEs and their effects on mental health (Oral et al., Reference Oral, Ramirez, Coohey, Nakada, Walz, Kuntz, Benoit and Peek-Asa2016; Bethell et al., Reference Bethell, Solloway, Guinosso, Hassink, Srivastav, Ford and Simpson2017; Srivastav et al., Reference Srivastav, Strompolis, Moseley and Daniels2020). The impact of ACEs may be worse in low-resource settings like Kenya due to limited mental health infrastructure and compounding socioeconomic stressors (Arena et al., Reference Arena, Adriani, Mancino, Sarno, Modesti, Del Casale and Ferracuti2025). Studies have shown that over 50% of Kenyan children and youth reported having experienced at least one ACE, with physical abuse, emotional neglect, and household dysfunction being the most prevalent. Additionally, children who were exposed to ACEs had a higher risk of developing mental health conditions like PTSD and depression (Miedema et al., Reference Miedema, Chiang, Annor and Achia2023; Ferrajão et al., Reference Ferrajão, Tourais, Faria, Dias and Elklit2024).
Individuals exposed to multiple ACEs are substantially more likely to experience suicidal ideations and behaviors (Angelakis et al., Reference Angelakis, Gillespie and Panagioti2019; Baiden et al., Reference Baiden, Antwi-Boasiako and den Dunnen2019; Burstein and Greenfield, Reference Burstein and Greenfield2020). In Kenya, young adults who experienced ACEs had significantly higher odds of poor mental health outcomes, including suicidal and self-harm behaviors, particularly among males (adjusted odds ratio = 6.7, 95% confidence interval [CI]: 2.8–16.0), highlighting ACEs as key contributors to youth suicidality in the country (Seya et al., Reference Seya, Matthews, Zhu, Brown, Lefevre, Agathis, Chiang, Annor, McOwen and Augusto2024). While resilience can mediate the relationship between ACEs and suicidality (Giovanelli et al., Reference Giovanelli, Mondi, Reynolds and Ou2020), its moderating function is still unclear (Zahradnik et al., Reference Zahradnik, Stewart, O’Connor, Stevens, Ungar and Wekerle2010).
Evidence also indicates that ACEs are a major predictor of PTSD (Bielas et al., Reference Bielas, Barra, Skrivanek, Aebi, Steinhausen, Bessler and Plattner2016), with 25–35% of children exposed to trauma and PTSD (John et al., Reference John, Russell and Russell2007; Wang et al., Reference Wang, Fu, Wu, Ma, Sun, Huang, Hashimoto and Gao2012). Nearly 50% of Nairobi high school pupils have been found to have PTSD (Ndetei et al., Reference Ndetei, Ongecha-Owuor, Khasakhala, Mutiso, Odhiambo and Kokonya2007), which is consistent with studies in Nigeria (Akinrogunde, Reference Akinrogunde2023) and Uganda (McMullen et al., Reference McMullen, O’Callaghan, Richards, Eakin and Rafferty2012). High levels of ACE exposure are also experienced by South African women, which may have an impact on the development of PTSD (Jewkes et al., Reference Jewkes, Dunkle, Nduna, Jama and Puren2010) and in Kenyan youth (Ferrajão et al., Reference Ferrajão, Tourais, Faria, Dias and Elklit2024).
ACEs have also been linked to depression (Turner et al., Reference Turner, Finkelhor and Ormrod2006; Bethell et al., Reference Bethell, Newacheck, Hawes and Halfon2014), with research from the United States, the United Kingdom, and Uganda demonstrating a robust correlation (Bellis et al., Reference Bellis, Lowey, Leckenby, Hughes and Harrison2014; Blum et al., Reference Blum, Li and Naranjo-Rivera2019; Elmore and Crouch, Reference Elmore and Crouch2020; Houtepen et al., Reference Houtepen, Heron, Suderman, Fraser, Chittleborough and Howe2020; Debowska et al., Reference Debowska, Boduszek, Fray-Aiken, Ochen, Powell-Booth, Nanfuka Kalule, Harvey, Turyomurugyendo, Nelson and Willmott2024). In Kenya, ACEs, especially sexual abuse, are linked to depressive symptoms in young people, highlighting the necessity of focused interventions (Mutamba, Reference Mutamba2020).
The role of resilience
Resilience is the ability to adapt positively to adversity, influenced by personal characteristics, family relationships, and more general social and environmental factors, and is associated with better mental health outcomes (Stainton et al., Reference Stainton, Chisholm, Kaiser, Rosen, Upthegrove, Ruhrmann and Wood2019; Ungar and Theron, Reference Ungar and Theron2020). Resilience is a key protective factor in mental health, with evidence suggesting that it can moderate and mediate the relationship between ACEs and mental health outcomes, and that resilient individuals exposed to ACEs exhibit lower rates of depression and suicidality (Poole et al., Reference Poole, Dobson and Pusch2017; Kelifa et al., Reference Kelifa, Yang, Herbert, He and Wang2020; Freeny et al., Reference Freeny, Peskin, Schick, Cuccaro, Addy, Morgan, Lopez and Johnson-Baker2021). Resilience serves as both a mediator and moderator in the relationship between ACEs versus suicidality and depression among youth (Rytilä-Manninen et al., Reference Rytilä-Manninen, Haravuori, Fröjd, Marttunen and Lindberg2018; Okwori, Reference Okwori2022). Ugandan studies found that resilience moderated the relationship between war-related trauma and suicidal ideation, indicating that fostering moderate resilience can reduce the likelihood of suicidal behaviors in this context (Haroz et al., Reference Haroz, Murray, Bolton, Betancourt and Bass2013; Okello, Reference Okello2014). A study in Germany revealed that social support enhances resilience, leading to better mental health outcomes among individuals with a history of ACEs (Wolff and Caravaca Sánchez, Reference Wolff and Caravaca Sánchez2019). Resilience has become a protective factor against the effects of trauma on mental health (Seery et al., Reference Seery, Holman and Silver2010; Poole et al., Reference Poole, Dobson and Pusch2017; Clements-Nolle and Waddington, Reference Clements-Nolle and Waddington2019). Moreover, this study is grounded in “ordinary magic” theory of resilience, which conceptualizes resilience as a common, adaptive process rooted in individual and contextual strengths (Michael Garrett, Reference Michael Garrett2016). In low-resource settings, resilience is often linked to familial and community factors rather than individual traits alone (Banyard et al., Reference Banyard, Rousseau, Shockley McCarthy, Stavola, Xu and Hamby2025). In Kenya, despite high rates of depression (Lawley, Reference Lawley2023), suicidal thoughts and intent (Leone, Reference Leone2024), and PTSD (Kaaria et al., Reference Kaaria, Nyagah and Ntarangwe2024), we have limited research investigating the mediating and moderating roles of resilience in the relationship between ACEs and mental health outcomes.
Mediation and moderation
Mediation and moderation analyses are necessary for discovering the relationship between ACEs, resilience, and mental health consequences. Mediation explains how resilience serves as a pathway through which ACEs influence mental health disorders, such as depression, PTSD, and suicidality (Panagou and MacBeth, Reference Panagou and MacBeth2022; Panagou, Reference Panagou2021), potentially lowering the risks by mitigating emotional dysregulation caused by trauma (Elrefaay and Elyzal, Reference Elrefaay and Elyzal2024). Moderation examines when and under what conditions resilience alters the strength or direction of the relationship between ACEs and these mental health outcomes (Zhang et al., Reference Zhang, Li, Jiang and Zhang2023), especially within high-risk environments (Okwori, Reference Okwori2022). Understanding and exploring these dynamics in Kenyan youth is crucial for finding potential cultural and contextual barriers and developing effective mental health interventions.
Knowledge gap
While previous studies have explored ACEs and the links between risk factors and their impact on mental health outcomes worldwide, research gaps still exist regarding how resilience mediates and moderates these relationships in the Kenyan context, and, in particular, no studies have compared how different categories of ACEs affect depression, PTSD, and suicidality.
General aim
The general aim is to investigate the association between the different categories of ACEs and suicidality, PTSD, and depression, and the moderating and mediating roles of resilience in the outcomes of the different categories of ACEs in the Nairobi Metropolitan Area.
Specific aims
-
1. To describe the distribution and correlations between ACEs, resilience, suicidal ideation and behavior, PTSD, and depression outcomes in Kenyan youth.
-
2. To assess the moderating effect of resilience on the relationship between ACEs and suicidality, PTSD, and depression outcomes.
-
3. To explore the mediating role of resilience in the relationship between ACEs, suicidality, PTSD, and depression outcomes.
-
4. To explore if our data can inform resilience interventions to mitigate the relationship between ACEs and the outcomes of suicidality, PTSD, and depression.
This study was guided by the following hypotheses
H1: Higher levels of ACEs will be significantly associated with increased depression, PTSD, and suicidal ideation and behavior in Kenyan youth.
H2: Resilience will moderate the relationship between ACEs and mental health outcomes (suicidality, PTSD, and depression).
H3: Resilience will mediate the relationship between ACEs and mental health outcomes (suicidality, PTSD, and depression).
H4: Patterns observed in the data will identify key resilience factors that can inform the development of interventions aimed at mitigating the effects of ACEs on suicidality, PTSD, and depression.
Methodology
Study design and setting
This was a cross-sectional study design conducted in Nairobi metropolitan capital city and Kiambu County (peri-urban). Participants from the community, high school level, and middle-level college located within the metropolitan area were recruited into the study.
Sampling
This study utilized a population-based convenience sampling technique. The inclusion criteria were all youths aged 14–25 years who were available, willing, and residing within the designated neighborhoods. While recruitment was not randomized, it was comprehensive and inclusive, leveraging local community leaders and school and college administrations to reach a broad cross-section of the population. The exclusion criteria were applied to individuals outside the designated age range and those unwilling to participate. Individuals incapable of comprehending the questionnaire due to factors such as intoxication or illiteracy were also excluded to minimize bias and incomplete data from self-report questionnaires.
Procedures
Research assistant (RA) selection and training
Twelve RAs selected through a competitive process underwent a 2-day comprehensive in-person training program that covered data collection techniques and procedures, including administering surveys. Additionally, they were trained on ethical procedures, such as obtaining informed consent and assent, ensuring confidentiality, and handling data accurately. The training also emphasized proper data handling, including real-time data verification, secure storage, and entry protocols to minimize errors. The program also included mock interviews to simulate real-world scenarios.
Recruitment and resulting sample
After receiving ethical approvals, we approached the County Commissioners in Kiambu and Nairobi Counties to explain to them the nature of the study and solicit their support. They then connected us with the chiefs and sub-chiefs who collaborated with community opinion leaders (elders) to sensitize and mobilize the youths in their areas. The chiefs, sub-chiefs, and elders were given a script that included information on the study, an invitation to the study at the designated time, date, and venue inside the study locations. They used it to actively engage through local meetings, community gatherings, and announcements at local centers, to organize and urge the youth to participate in the study. English literacy was a requirement for participation since all the questionnaires were administered in English in this context. While these criteria may limit the generalizability of findings to all youth, nobody met this exclusion criterion. However, chiefs’ and sub-chiefs’ ability to speak English was not a criterion for youth participation, as communication with potential participants was handled directly by the RAs. We assigned a number (1–12) per RA, with each number forming a distinct group. Participants were then assigned to the group in a restricted randomization, where a printed voucher with numbers 1–12 on each page was used. This ensured balanced group sizes and facilitated smooth distribution of the questionnaires, as well as efficient and simultaneous data collection across groups. Each group comprised a maximum of 25 participants and was led by the respective RA assigned to that group. The RAs distributed questionnaires, verified ages, and collected written informed consent and assents. To ensure standardization, participants responded to the questions based on their understanding, thereby minimizing any potential influence from external assistance.
A total of 1,972 participants participated in the study. RAs explained the study’s goals, methods, risks, rewards, and confidentiality. Participants had the right to withdraw without facing consequences before providing their consent. None of the participants declined participation. Adults affirmed their voluntary participation as per ethical guidelines by signing informed consent and assent for those below 18 years, which is the legal age in Kenya for minors. Minors were accompanied by a parent or a legal guardian for consent only, but completed the questionnaires independently, with guardians not permitted in the data collection area. Refunds were made for any travel expenses or lost income during their participation, and snacks were provided.
Data collection
All the data were collected during the day from September 21, 2022, to December 15, 2022. Data were collected on sociodemographics, ACEs, suicidality, depression, PTSD, and resilience. Participants completed self-administered questionnaires confidentially in group settings within social halls, similar to an exam environment where no communication occurs among participants. Additionally, to ensure privacy, each participant was provided with sufficient space to fill out the questionnaire without being able to see the responses of others to minimize social desirability bias. Students used school/college halls, while community participants used public halls in Nairobi and Kiambu that were approved for research purposes.
Instruments
Sociodemographic profile
-
a. We collected data on age, gender, marital status, religion, birth position, level of education, employment status, primary source of income, place of abode, and whether they were sharing the living space(s).
-
b. Wealth Index: This was developed by the World Bank for use in low- and middle-income countries (LMICs) and uses household items to determine family socioeconomic status. It was constructed using principal component analysis based on the Demographic Health Survey model, assessing socioeconomic data on household assets, water sources, floor type, toilet facilities, and primary fuel sources for cooking (McLorg et al., Reference McLorg, Omolo, Sifuna, Shaw, Walia and Larsen2021). The Wealth Index is classified from high to low on a 5-point Likert scale (Rutstein, Reference Rutstein2015).
Adult resilience measure-revised (ARM-R)
The ARM-R is a self-report questionnaire designed to assess resilience from a socio-ecological lens (Liebenberg and Moore, Reference Liebenberg and Moore2018; Jefferies et al., Reference Jefferies, McGarrigle and Ungar2019; Resilience Research Centre, 2022). The ARM-R instrument consists of 17 items capturing the protective factors at the individual, relational, and community levels, scored on a 5-point Likert-type scale ranging from 1 = “Not at all” to 5 = “A lot”. The ARM-R measures the capacity to access resources in an individual’s environment (personal resilience) and the extent to which social entities in the environment (e.g., family, peers, and institutions) provide resources (relational resilience). All items in the questionnaire are positively worded, facilitating straightforward scoring by summing up the scores directly. Total resilience scores range from 17 to 85, with higher scores indicating greater resilience. Developed through a cross-cultural exploration involving 14 communities across 11 countries worldwide (Ungar et al., Reference Ungar, Liebenberg, Boothroyd, Kwong, Lee, Leblanc, Duque and Makhnach2008), the ARM-R demonstrates good psychometric properties, including strong internal reliability/consistency, content, and face validity, and is used worldwide, that is, in Syria (Ipekci, Reference Ipekci2021) and Brazil (Ferreira et al., Reference Ferreira, Bezerra, de Lima, Jefferies, Coimbra, da Cunha, Santos, da Silva, Brasil and Ungar2022) and across cultures in diverse studies of resilience (Ungar et al., Reference Ungar, Liebenberg, Boothroyd, Kwong, Lee, Leblanc, Duque and Makhnach2008; Jefferies et al., Reference Jefferies, McGarrigle and Ungar2019). We examined scale reliability using Cronbach’s α for the 17 items of the ARM-R and found that the α > 0.80, indicating good consistency (DeVellis, Reference DeVellis1991). The Cronbach’s αfor 16 years and above was 0.904, and that for <16 years was 0.898, indicating its reliability in this age group in our study (Zrihan-Weitzman et al., Reference Zrihan-Weitzman, Merhav, Farchi and Peled-Avram2023).
The traumatic and distress scale (TADs)
The TADS, a self-report questionnaire, was used for the assessment of multiple types of ACEs (Salokangas et al., Reference Salokangas, Schultze-Lutter, Patterson, von Reventlow, Heinimaa, From, Luutonen, Hankala, Kotimäki and Tuominen2016). ACEs such as abuse and neglect were evaluated using the TADS items, which measure experiences across five main domains, namely emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect, each comprising five items. Each item is rated on a 5-point Likert scale from 0 to 4 (0 = never, 1 = rarely, 2 = sometimes, 3 = often, and 4 = nearly always). We explored the five TADS domains for ACEs. The TADS has excellent internal consistency within each domain and establishes its validity, reliability, and clinical utility in retrospectively assessing childhood traumatization (Salokangas et al., Reference Salokangas, Schultze-Lutter, Patterson, von Reventlow, Heinimaa, From, Luutonen, Hankala, Kotimäki and Tuominen2016). The TADS total score, indicative of the overall extent of childhood trauma, was calculated as the total score of all five domains (De Venter et al., Reference De Venter, Illegems, Van Royen, Sabbe, Moorkens and Van Den Eede2020; Salokangas et al., Reference Salokangas, Schultze-Lutter, Schmidt, Pesonen, Luutonen, Patterson, von Reventlow, Heinimaa, From and Hietala2020). The internal reliability using Cronbach’s α for all the 43 TADS items and 25 items for the ACEs domain was calculated and found to be good (α = 0.880 and α = 0.850, respectively).
The Columbia–suicide severity rating scale (C-SSRS)
We assessed suicidal ideations and behaviors based on self-reported C-SSRS (Posner et al., Reference Posner, Brown, Stanley, Brent, Yershova, Oquendo, Currier, Melvin, Greenhill and Shen2011). Indeed, C-SSRS does not introduce new criteria for suicidality and, at best, brings all of them into one tool. The C-SSRS has been validated in a study of the Lebanese population, indicating its applicability in a variety of LMIC contexts, despite the lack of research on suicidality assessment instruments in these contexts (Zakhour et al., Reference Zakhour, Haddad, Sacre, Fares, Akel, Obeid, Salameh and Hallit2021). It measures four constructs to distinguish between the domains of suicidal ideation and behavior. The “severity subscale” measures the severity of ideation using a 5-point ordinal scale ranging from 1 (wish to be dead) to 5 (suicidal intent with a plan). The “intensity subscale” consists of five items, each rated on a 5-point ordinal scale, assessing frequency, duration, controllability, deterrents, and reason for ideation. The “behavior subscale” includes categories such as actual, aborted, and interrupted attempts, preparatory behavior, and nonsuicidal self-injurious behavior. The “lethality subscale” rates actual attempts on a 6-point ordinal scale, with potential lethality rated if actual lethality is 0. Psychometric evaluations have consistently demonstrated the scale’s reliability, internal consistency, and construct validity, with evidence supporting its ability to accurately predict suicide risk across different populations (Yershova et al., Reference Yershova, Lesser, Logan and Posner2016; Austria-Corrales et al., Reference Austria-Corrales, Jiménez-Tapia, Astudillo-García, Arenas-Landgrave, Xochihua-Tlecuitl, Cruz-Cruz, Rivera-Rivera, Gómez-García, Palacios-Hernández and Pérez-Amezcua2023; Schwartzman et al., Reference Schwartzman, Muscatello and Corbett2023). We examined the internal consistency of the C-SSRS Cronbach’s α, and found the internal consistency for lifetime and recent versions was α = 0.821 and α = 0.801, respectively, which demonstrated good reliability.
Post-traumatic stress disorder
The Harvard Trauma Questionnaire (HTQ) is a four-part instrument that focuses on (i) experiences of torture and other traumas frequently experienced; (ii) a subjective description of the most severe traumatic event(s) experienced; (iii) events associated with head injuries; and (iv) symptoms of PTSD and expressions of functional distress. It was developed in the early 1990s as a cross-cultural screening instrument to document trauma exposure, head trauma, and trauma-related symptoms. While the original tool focused on refugee segments (Indo-Chinese refugee populations), where it exhibited strong psychometric properties, it is increasingly being used in other contexts, including low-prevalence community samples (Mollica et al., Reference Mollica, Caspi-Yavin, Bollini, Truong, Tor and Lavelle1992). It has since been translated and validated in several languages for many regions and population samples (Halepota and Wasif, Reference Halepota and Wasif2001; Lhewa et al., Reference Lhewa, Banu, Rosenfeld and Keller2007; Oruc et al., Reference Oruc, Kapetanovic, Pojskic, Miley, Forstbauer, Mollica and Henderson2008; de Fouchier et al., Reference de Fouchier, Blanchet, Hopkins, Bui, Ait-Aoudia and Jehel2012). The first 16 items were derived from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria for PTSD. The DSM-IV PTSD score is calculated from the first 16 items. The higher the scores on the DSM-IV PTSD items, the more likely it is that the respondent will have a PTSD diagnosis. Response options were “yes” and “no.” Cumulative trauma exposure scores were calculated by a count of “yes” responses to all items.
Patient Health Questionnaire-9
The PHQ-9 is a nine-item self-report questionnaire designed to measure depression (Kroenke and Spitzer, Reference Kroenke and Spitzer2002). Items are rated on a 4-point Likert scale, ranging from 0 (not at all) to 3 (nearly every day). The cumulative score can range from 0 to 27, with higher scores indicative of more pronounced depression. The questions address sleep, energy, appetite, and other possible symptoms of depression by asking respondents how often they have “been bothered by any of the following problems” in the past 2 weeks. Originally validated in the United States, the PHQ-9 demonstrates robust psychometric properties and has been extensively employed in culturally diverse settings (Kroenke et al., Reference Kroenke, Spitzer and Williams2001). Interpretation of the total score categorizes depression severity into minimal (0–4), mild (5–9), moderate (10–14), moderately severe (15–19), or severe (20–27) categories. The nine items of the PHQ-9 demonstrated good internal consistency in this study, with Cronbach’s α of 0.814, indicating a reliable measure of depressive symptoms.
Ethics
All procedures involving human subjects/patients were approved by the Nairobi Hospital Ethics Research Committee (Approval no. TNH-ERC/DMSR/ERP/022/22). The study obtained licensing from the National Commission for Science, Technology, and Innovation (NACOSTI) license NACOSTI/P/22/18097. Administrative permissions were sought from the county-level offices in Kiambu and Nairobi counties to allow engagement with community participants. Additionally, institutional approval from the colleges was obtained, as data collection involved students, ensuring compliance with institutional policies on research involving students. Informed written consent/assent was obtained from the participants before data collection commenced. For participants younger than the age of 18 years, informed written consent to participate was obtained from their parents or legal guardians.
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences (IBM SPSS version 25). Descriptive statistics were done to summarize the mean scores of ACEs, PTSD, depression, resilience, and suicidality. We utilized Spearman’s rank correlation to evaluate the correlation between ACEs, resilience, depression, PTSD, and suicidality because it is robust to deviations from normality and effectively captures both linear and monotonic relationships. In mediation and moderation analysis, Hayes’ SPSS Process Macro (version 4.2 beta) was used with ACEs as predictors and depression, PTSD, and suicidal ideation and behavior as dependent variables. Resilience was incorporated as both a moderator and mediator because of its recognized theoretical function in mitigating the psychological effects of ACEs, as it is seen as a critical component in improving coping strategies and lowering emotional discomfort (Morgan et al., Reference Morgan, Chang, Choy, Tsai and Hsieh2021).
Moderation: An interaction term (ACEs × Resilience) was included in a regression model to assess whether resilience alters the strength of the relationship between ACEs and psychological outcomes. Mediation: Regression-based path analysis was conducted, exploring both the direct and indirect effects of ACEs on depression, PTSD, and suicidal ideation and behavior through resilience. CIs based on bootstrapping were applied to enhance the accuracy of identifying indirect effects, ensuring that this method is both robust and reliable. A significance level of p < 0.05 was used for all analyses, and effect sizes with 95% CIs were reported to evaluate the strength and robustness of the relationships. Hayes’ Process Macro was chosen for its ability to simultaneously evaluate moderation and mediation effects, offering a comprehensive framework for analyzing both direct and complex indirect relationships (Hayes, Reference Hayes2018). The statistical assumptions for regression-based analyses, including linearity, homoscedasticity, and multicollinearity, were assessed before conducting the analyses. The variance inflation factors and tolerance values for the predictor, moderator, and mediator variables were below 10 and above 0.1, respectively, indicating no multicollinearity concern. In all the analyses, scores were treated as continuous variables to retain variability and statistical power (Wu and Leung, Reference Wu and Leung2017). Higher scores indicated higher experiences or symptoms.
Results
Social demographics
The study included 1,972 participants (55% female, mean age = 20.49 ± 2.63, range = 14–25 years). Most participants were from urban settings (91.5%), were Christians (87.2%), and were unmarried (60.4%). The unemployment rate was high (77.9%) since most participants were in school. More than half (53.1%) were in the lowest quintiles (1 and 2) (Table 1).
Table 1. Social demographics

Note: The Wealth Index was constructed using the DHS standard and utilized the socioeconomic data on assets and utilities.
Descriptive statistics and correlations for ACEs, resilience, depression, suicidal ideation and behavior, and PTSD
There were higher levels of negligence than abuse among the participants. All five ACEs are positively correlated to one another, as well as with PTSD (r = 0.101–0.205, p < 0.05) and depression (r = 0.101–0.389, p < 0.05). Resilience was negatively correlated with PTSD (r = −0.141, p < 0.05), depression (r = −0.361, p < 0.05), suicidal behavior (recent) (r = −0.198, p < 0.05), and suicidal ideation (recent) (r = −0.187, p < 0.05). Additionally, PTSD and depression were positively correlated (r = 0.332, p < .05), as were depression and suicidal ideation lifetime (r = 0.302, p < 0.05) (Table 2).
Table 2. Descriptive statistics (mean and standard deviations) and correlations for ACEs, depression, resilience, PTSD, suicide ideations and behavior

Note: SD, standard deviation. The correlations show the strength and direction of relationships between the variables. The correlation marked (**) indicates significance at p < 0.05.
Moderation analysis
Resilience as a moderator between ACEs and PTSD, depression, and suicidality (ideation and behavior)
Resilience had a significant negative relationship with all three outcomes (p < 0.05), affirming its protective role. The associations of interactions show a complex dynamic (Table 3):
-
• PTSD: Resilience moderated the association of emotional and physical negligence and sexual abuse on PTSD. Higher resilience lowers the negative influence of ACEs on PTSD symptoms (p < 0.05).
-
• Depression: Resilience acted as a buffer against depression, showing significant negative associations across ACE domains, such as emotional and physical negligence (p < 0.05).
-
• Suicidality: Emotional negligence (β = 0.0022, p = 0.0059) and physical negligence (β = 0.0026, p = 0.0179) showed a significant interaction effect on lifetime suicidal ideation. Additionally, resilience showed a borderline significant moderation for physical abuse on lifetime suicidal behavior (β = −0.0024, p = 0.0479) and recent suicidal behavior (β = −0.0017, p = 0.05) and total ACEs on recent suicidal behavior (β = −0.0004, p = 0.0514).
Table 3. Resilience as a moderator between ACES and PTSD, depression (PHQ-9), suicidal ideations, and behavior
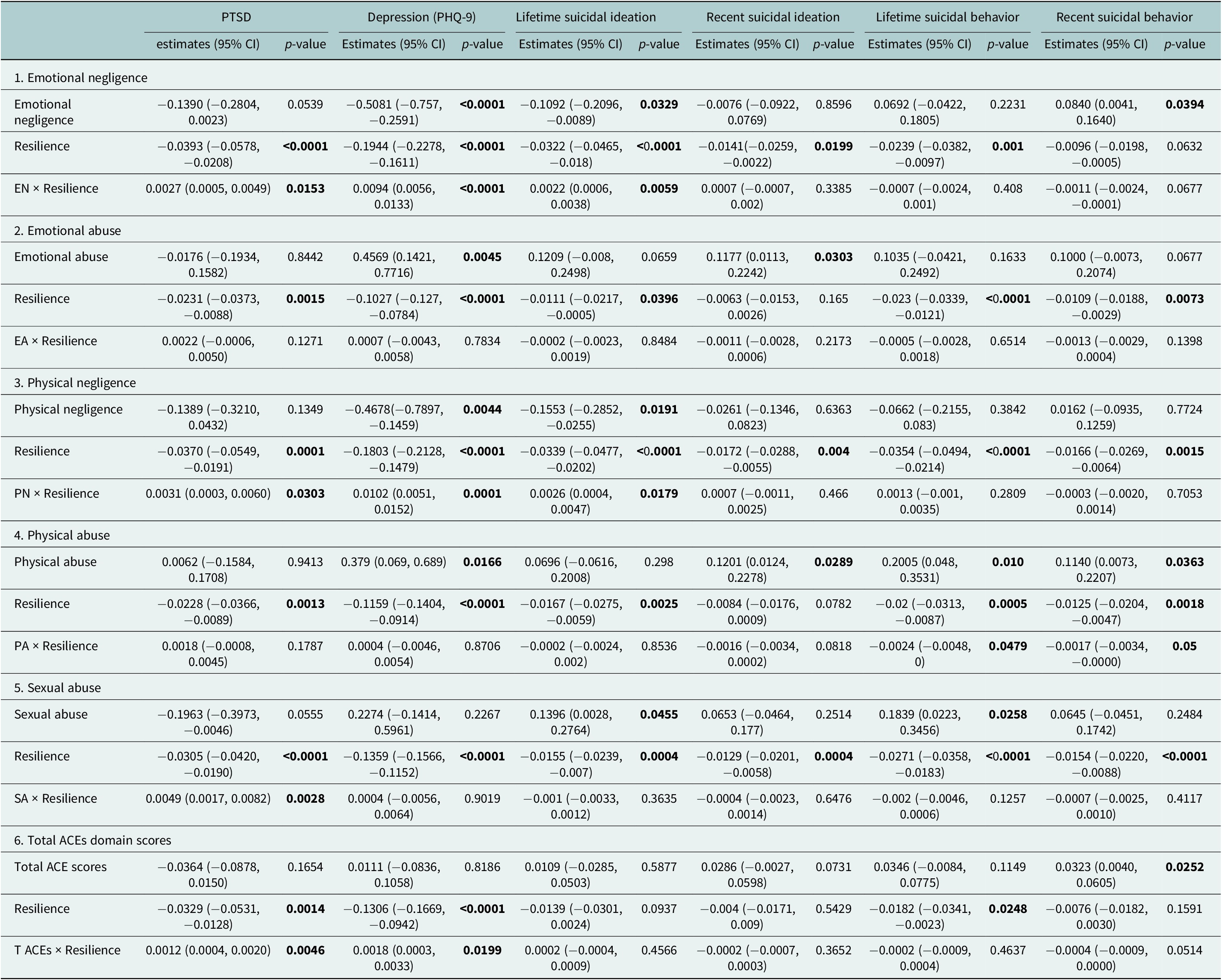
Note: EA, emotional abuse; EN, emotional negligence; PA, physical abuse; PN, physical negligence; SA, sexual abuse; TACEs, total ACE scores. Dependent variables are PTSD, depression (PHQ-9), and suicidal ideation and behavior assessed across lifetime and recent. Predictor variables include emotional/physical/sexual neglect or abuse, total ACEs domain scores, and resilience. Estimates (95% CI): The regression coefficients representing the relationship between the predictor variable and the outcome variable, along with the 95% confidence interval (CI). In some models, ACEs appear to be negatively associated with outcomes due to variable centering and interaction inclusion. These should not be interpreted as protective effects. Rather, they reflect conditional associations at average resilience levels. The interaction term often captures the key variance when moderation is present and does not contradict the established positive link between ACEs and poor mental health. Interaction terms (ACEs × Resilience) should be interpreted in context. When the main effect of ACEs is positive, a negative interaction indicates that resilience buffers the risk, while a positive interaction suggests amplification. When the main effect is negative, a positive interaction weakens that effect (possibly protective), and a negative interaction strengthens it (possibly harmful). The significant p-values are bolded.
Mediation analysis
Pathways from ACEs to resilience to depression, PTSD and suicidality ideation and behavior
We report standardized β-coefficients for key paths in the moderation and mediation models, which ranged from small to medium effect sizes (Table 4).
-
• ACEs and PTSD through resilience: Resilience partially mediated the relationship between most ACEs (direct and indirect effects; p < 0.05) and PTSD symptoms. However, for the total ACE score, the indirect effect on PTSD was nonsignificant (p > 0.05), indicating no mediation. Emotional negligence demonstrated complete mediation, as resilience absorbs the entire effect (indirect effect significant and direct effect nonsignificant).
-
• ACEs and depression through resilience: While all ACE domains showed significant direct and indirect effects (partial mediation), emotional and physical abuse revealed the strongest direct effects, underscoring resilience’s partial mediation across most domains.
-
• ACEs and suicide ideation through resilience: Resilience partially mediated the relationship between ACEs and lifetime/recent suicide ideation for most ACE domains. However, emotional and physical negligence demonstrated complete mediation for lifetime ideation, while for recent suicidal ideation, resilience fully mediated the effects of physical abuse and negligence, while partial mediation was observed for all other ACEs, suggesting resilience can entirely offset the adverse impacts of these ACEs on ideation.
-
• ACEs and suicide behavior through resilience: Resilience fully mediated the effects of ACEs on suicidal behaviors for most domains (p < 0.001, indirect effects, nonsignificant direct effects). Partial mediation is observed for ACE domains, such as emotional, physical, and sexual abuse, in relation to lifetime suicidal behavior.
Table 4. Mediation analysis: Examining how ACEs associate with mental health outcomes (PTSD, depression, suicidal ideation and behavior) both directly and indirectly through resilience

Note: Dependent variables: PTSD, depression, lifetime and recent suicidal ideations and behavior. Mediator (resilience). Independent variables (ACEs). Total effect: The “total effect of ACEs on the dependent variable” represents the combined direct and indirect effects of ACE on the dependent variable. Direct effect: The “direct effect of ACEs on the dependent variable” is the effect of ACE on the dependent variable when resilience is not considered. Indirect effect: The “indirect effect of ACE on the dependent variable through resilience” represents the mediated effect of ACE on the dependent variable through the mediator “Resilience.” The significant p-values are bolded.
Discussion
Our study presents a comprehensive investigation in Kenya of the link between different categories of ACEs and depression, suicidality, and PTSD, with consideration of the role of resilience as a mediator or moderator in youth living in the Nairobi Metropolitan Area. We found a strong correlation (ACEs and symptoms of depression, PTSD, and suicidality). The relationship between ACEs and depression and PTSD was significantly moderated by resilience and partially mediated by resilience, indicating a role in protecting the mental health of Kenyan youth. While findings may offer insights relevant to similar urban and peri-urban youth settings in Kenya and comparable low-resource contexts, the nonrandom sampling approach limits broader generalizability. We stress that resilience is crucial in mitigating these negative effects of ACEs on outcomes and advocate for its integration into interventions.
Social demographics
All the participants were in their youth (up to 25 years). The majority lived in the urban area where most of our research sites were located; there were more females than males, which reflects increased enrollment of females in schools, an emerging observation in the Kenyan education system. Most were Christians, which is the predominant religion in Kenya, and most were unmarried since they were students and came from a lower socioeconomic status.
Moderation and mediation interpretations
ACEs, mental health (PTSD, suicidality, and depression), and the role of resilience
Our findings align with previous global and regional studies, which showed a direct positive relationship between ACEs and adverse mental health outcomes (PTSD, suicidality, and depression) (Ndetei et al., Reference Ndetei, Ongecha-Owuor, Khasakhala, Mutiso, Odhiambo and Kokonya2007; Jewkes et al., Reference Jewkes, Dunkle, Nduna, Jama and Puren2010; McMullen et al., Reference McMullen, O’Callaghan, Richards, Eakin and Rafferty2012; Bielas et al., Reference Bielas, Barra, Skrivanek, Aebi, Steinhausen, Bessler and Plattner2016; Angelakis et al., Reference Angelakis, Gillespie and Panagioti2019; Baiden et al., Reference Baiden, Antwi-Boasiako and den Dunnen2019; Blum et al., Reference Blum, Li and Naranjo-Rivera2019; Houtepen et al., Reference Houtepen, Heron, Suderman, Fraser, Chittleborough and Howe2020; Debowska et al., Reference Debowska, Boduszek, Fray-Aiken, Ochen, Powell-Booth, Nanfuka Kalule, Harvey, Turyomurugyendo, Nelson and Willmott2024; White et al., Reference White, Prasad, Ammar, Yaun and Shaban-Nejad2024). Further, we found that Kenyan youth exposed to ACEs exhibited high levels of depressive symptoms, with resilience that negatively correlated with both ACEs and depression, as has been found in other countries (Abbott and Slack, Reference Abbott and Slack2021; Girma et al., Reference Girma, Tsehay, Mamaru and Abera2021).
In relation to the three mental health outcomes in our study, resilience serves as a mediator and a moderator, although to varying degrees, and all agree with the global literature summarized under the Introduction section:
-
i. Moderating role: While resilience moderated the effects of ACEs on depression and PTSD, there are conflicting results in suicidality. Resilience moderated specific ACE-suicidality links, including neglect, abuse, and total ACEs, but was less protective in cases involving emotional or sexual abuse.
-
ii. Mediating role: The connection between ACEs and the three mental health outcomes was largely mediated by resilience, except for emotional neglect, where it fully mediated suicidality and PTSD. This implies that emotional neglect may have a greater impact on mental health through pathways linked to resilience than through actual psychological discomfort.
These findings emphasize the necessity of adjusting resilience-building interventions to certain ACE types, acknowledging that certain adversities can call for more involved or specialized methods. Those in violent and aggressive families are prone to PTSD, coupled with cultural beliefs and practices that tolerate and accept family violence and physical punishment, as was found by Fulu et al. (Reference Fulu, Miedema, Roselli, McCook, Chan, Haardörfer, Jewkes, Warner, Lang and Naved2017). Emotional and physical neglect, the most frequent ACEs, impede stress buffering and the development of secure attachment, increasing PTSD, as found by Margolin and Vickerman (Reference Margolin and Vickerman2007) and Spinazzola et al. (Reference Spinazzola, Hodgdon, Liang, Ford, Layne, Pynoos, Briggs, Stolbach and Kisiel2014).
It is noteworthy that resilience negatively correlates with ACEs and PTSD, suggesting that individuals with higher resilience levels are less susceptible to PTSD symptoms. This concurs with similar findings (Reich et al., Reference Reich, Zautra and Hall2010; Biggs et al., Reference Biggs, Seech, Johnston and Russell2024). Notably, resilience moderates the relationship between ACEs and PTSD, particularly in mitigating the association of emotional and physical negligence and sexual abuse. These results align with existing literature, which underscores the importance of resilience as a protective factor against PTSD (Seery et al., Reference Seery, Holman and Silver2010; Rutter, Reference Rutter2013). Additionally, resilience partially mediated the relationship between all ACEs and PTSD symptoms, except emotional neglect, where it fully mediated this relationship, which aligns with the findings of previous studies (Guo et al., Reference Guo, Huang, Hall, Jiao, Chen, Yu, Yeung, Chi and Zou2021).
Resilience moderated the relationship between emotional and physical negligence with lifetime and recent suicidal ideation in agreement with studies from China and the United States, which emphasize resilience as a key factor in reducing the risk of suicidality in individuals exposed to ACEs (Thompson et al., Reference Thompson, Kingree and Lamis2019; Yu et al., Reference Yu, Wang, Chen, Perrin and Gross2021). However, resilience did not significantly moderate the effects of emotional and sexual abuse on suicidal behaviors, highlighting the variability in its protective effects across different types of ACEs, as has been found in other studies (Brodsky and Stanley, Reference Brodsky and Stanley2008; Dahlby, Reference Dahlby2022). Notably, resilience demonstrated minimal moderating effects on suicidality, particularly for emotional and sexual abuse, suggesting that suicidality may operate through distinct pathways less responsive to general resilience mechanisms. For example, acute life stressors, perceived burdensomeness, thwarted belongingness, or the lack of care and peer support may have more immediate effects on suicidal thoughts and behavior (Glenn et al., Reference Glenn, Kleiman, Kandlur, Esposito and Liu2022). In addition, development and psychosocial pathways to suicidality may differ from PTSD and depression and thus may require other protective mechanisms, such as emotional regulation, connectedness, or specific cognitive coping strategies (Sher, Reference Sher2019). These distinctions imply that ACEs measured in this study may not be sufficient to buffer the effect of ACEs on suicidality alone and suggest that there is a need for more specific interventions that address the suicide-specific risk and protective factors. Pathways showing full mediation, such as emotional neglect leading to PTSD or suicidality, may reflect resilience mechanisms like emotional regulation and perceived support, which are more directly disrupted by neglect. In contrast, partial mediation in abuse-related pathways suggests additional unmeasured factors – such as trauma severity or interpersonal betrayal – may also influence outcomes beyond what resilience alone can buffer. The nonsignificant moderation effect of resilience on suicidality may suggest that suicidal ideation in this context is less influenced by internal coping mechanisms and more shaped by external stressors or acute trauma. Future studies should explore additional moderators such as peer support or access to mental health care. The observed partial mediation suggests that while resilience explains part of the relationship between ACEs and mental health outcomes, other pathways are also at play. This is consistent with ecological systems theory, which posits that individual outcomes are shaped by multiple interacting influences. Furthermore, resilience acted as both a partial and complete mediator in the relationship between ACEs and suicidal ideation or behaviors, depending on the type of adversity, which agrees with the prior study (Giovanelli et al., Reference Giovanelli, Mondi, Reynolds and Ou2020). For instance, resilience fully mediated the effects of emotional negligence on recent suicidal ideation while partially mediating the effects of emotional abuse, physical abuse, and sexual abuse (p < 0.001).
Resilience significantly moderates the relationship between ACEs and the PHQ-9 assessment tool. This suggests that the relationship between these ACEs and depression was much more pronounced in people with lower resilience levels, which agrees with prior literature (Poole et al., Reference Poole, Dobson and Pusch2017). Moreover, our findings show that resilience partially mediated the relationship between depression and ACEs, indicating that while it reduces the adverse effects of childhood adversity, it does not eliminate them. This aligns with broader research highlighting resilience as a critical but insufficient factor in addressing mental health outcomes related to ACEs (Luthar and Zelazo, Reference Luthar and Zelazo2003; Clements-Nolle and Waddington, Reference Clements-Nolle and Waddington2019).
Comparison with regional and global literature
Our findings are consistent with other international studies, which found that resilience-building interventions yield substantial mental health benefits for clients who experienced childhood adversity (Malhi et al., Reference Malhi, Das, Bell, Mattingly and Mannie2019; Ungar and Theron, Reference Ungar and Theron2020). Moreover, our findings align with regional studies in sub-Saharan Africa, such as Kenya (Mwiti, Reference Mwiti2024) and Rwanda (Satinsky et al., Reference Satinsky, Kakuhikire, Baguma, Rasmussen, Ashaba, Cooper-Vince, Perkins, Kiconco, Namara and Bangsberg2021), which also found ACEs to be significantly associated with poor mental health outcomes. However, consistent with global research, resilience emerged as a protective factor across settings.
Implications and recommendations
The implications and recommendations from our findings are that developing early prevention interventions like school-based programs, community-driven approaches, and policy-level interventions could prevent or lessen PTSD, suicidality, and depression among Kenyan youth, especially in impoverished and high-crime regions, which are observed in the Nairobi metropolitan area (Ndetei et al., Reference Ndetei, Ongecha-Owuor, Khasakhala, Mutiso, Odhiambo and Kokonya2007; Vundi, Reference Vundi2022). Moreover, our results point to the protective role of resilience, but it is important that interventions tackle not only the consequences of ACEs (resilience) but also the root causes of mental health problems. Early identification of at-risk children, prevention through trauma-informed care, as well as community-based interventions aimed toward the perpetuating factors of ACEs, poverty, violence, and parental neglect need to be the focus of prevention efforts. However, resilience-building programs should not be used to replace the prevention of ACEs.
Limitations and future directions
Cross-sectional data limits causal inference when conducting mediation and moderation analysis. Without repeated measures over time, it is not possible to determine the directionality of the relationships examined. Also, moderation analysis detects interaction effects at one point in time, yet it fails to prove which event occurs first or second between the moderator and exposure or outcome. Future studies would benefit from longitudinal approaches to examine how ACEs affect and the protective role and resilience evolve over time. They could provide insight into causal pathways and aid in timely intervention decisions for longitudinal data. While the use of convenience sampling may limit the generalizability of the findings to broader youth populations beyond the study areas, the selected sites were nonetheless representative of Kenyan youth. The English literacy requirement may have introduced selection bias by excluding less educated or marginalized youth. This could have limited the generalizability and potential skewness of findings toward more advantaged, resilient participants.
Additionally, self-report measures may introduce recall and social desirability bias. Future research should employ longitudinal controlled studies and potentially bias-free objective measures to strengthen the validity of findings. Also, guardian presence may have caused underreporting of sensitive issues, introducing social desirability bias and underestimating ACEs’ impact. Finally, the use of HTQ may not align with DSM-5 or capture culturally specific trauma symptoms among Kenyan youth in community settings. Future research should use culturally adapted, updated tools for trauma assessment.
Conclusions
We conclude that our findings underscore the critical role of resilience-building interventions in mitigating the impact of ACEs on suicidality, particularly in resource-constrained settings like Nairobi. A similar conclusion was reached by other studies (Al-Sabah et al., Reference Al-Sabah, Legerski, Layne, Isakson, Katalinski, Pasalic, Bosankic and Pynoos2015; Hamby et al., Reference Hamby, Elm, Howell and Merrick2021; Morgan et al., Reference Morgan, Chang, Choy, Tsai and Hsieh2021). Our research sheds important light on the complex relationships that exist between ACEs, resilience, and the three studied mental health outcomes in young people in Kenya, thereby addressing the knowledge gap and fulfilling our general objective and specific aims, and in the process providing positive answers to all our research questions. There is a necessity for resilience-focused interventions that are customized to each of the three mental health outcomes and adversity. The interventions should build resilience via school mental health programs, trauma-informed teaching, peer support, and counseling. Engaging caregivers and elders while honoring Kenyan cultural values like collectivism and religious coping enhances impact. Kenya may significantly reduce the long-term effects of childhood trauma on mental health by incorporating resilience-building techniques frameworks in educational institutions in the community and supported by appropriate policy to achieve better mental outcomes in mental disorders in our study. These interventions can be implemented by trained nonmental health specialists and, in the process, achieve critical reach. Hence, reducing the risk of mental health disorders in Kenyan youth involves preventing ACEs and promoting resilience. All interventions must be holistic and take into consideration adverse environments while also teaching youth psychological tools to cope with adversity.
Open peer review
To view the open peer review materials for this article, please visit http://doi.org/10.1017/gmh.2025.10041.
Data availability statement
Requests for the data may be sent to the corresponding author.
Author contribution
D.M.N.: conceptualization and drafting of the paper. V.M.: oversight of data collection. C.M.: oversight of ethics. E.J.: statistical analysis and literature review. P.N.: draft review. S.W.: statistical analysis. V.O.: field work during data collection and literature review. K.B.: critique of the manuscript. D.M.: conceptualization and critique of the manuscript. All authors read and approved the final manuscript.
Financial support
This study was funded by the National Institutes of Health (NIH), grant/award number: 5R01MH127571-02.
Competing interests
The authors declare none.
Ethics statement
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human subjects/patients were approved by the Nairobi Hospital Ethics Research Committee (approval no. TNH-ERC/DMSR/ERP/022/22). The study obtained licensing from the National Commission for Science, Technology, and Innovation (NACOSTI) license NACOSTI/P/22/18097. Informed written consent/assent was obtained from participants before data collection commenced. For participants younger than the age of 18 years, informed written consent to participate was obtained from their parents or legal guardians.







