Across Australian public and private healthcare facilities, hip, knee, and shoulder arthroplasties accounted for 122,500 surgical procedures in 2018.1 As Australia’s population ages, the need for joint replacement procedures increase. Recent epidemiological modeling of the Australian Orthopaedic Association National Joint Replacement Registry (AOANJJR) dataset over 10 years (2003–2013) estimates the incidence of total knee joint replacement (TKJR) and total hip joint replacement (THJR) for osteoarthritis to increase by 276% and 208%, respectively, by 2030, with a total cost to the healthcare system estimated at AUD 5.32 billion (US$3.7 billion).Reference Ackerman, Bohensky and Zomer2 When complications such as prosthetic joint infections arise, the estimated cost of admission is ~3.1 times greater than that of a primary arthroplasty.Reference Peel, Dowsey and Buising3 Thus, prevention of infection in high-volume orthopedic procedures is warranted to improve patient care and costs to the healthcare system.
Reflective of these high volumes, audits of surgical antimicrobial prophylaxis (SAP) commonly target orthopedic surgical procedures in Australia4–6 and internationally.Reference Ou, Jing and Guo7–Reference Pittalis, Ferraro and Piselli9 The Australian Surgical National Antimicrobial Prescribing Survey (Surgical NAPS) was developed to facilitate and standardize SAP auditing via the collection of surgery details and timing of antimicrobials for benchmarking and targeted feedback of SAP prescribing.4,6 The Surgical NAPS report revealed that orthopedics is the most commonly audited surgical procedure group, accounting for 1,294 of all 4,674 procedural doses (27.7%) and 824 of 1,973 postprocedural SAP prescriptions (41.8%).6 A recent analysis of the Surgical NAPS data through June 30, 2018, revealed high rates of inappropriate SAP prescribing or orthopedic procedures.Reference Ierano, Thursky and Marshall10 When taking into account a range of hospital, patient, and surgical factors, SAP appropriateness for orthopedic procedures was low across procedural prescriptions (39.5%) and postprocedural prescriptions (53.0%).Reference Ierano, Thursky and Marshall10 Current national guidelines (ie, Therapeutic Guidelines: Antibiotic 12) recommend a preprocedural single-dose SAP for some procedures, (eg, prosthetic large joint replacements), but not all procedures require SAP (eg, arthroscopy without implantation of prosthetic material).Reference Berríos-Torres, Umscheid and Bratzler11,12
The guidelines acknowledge the lack of evidence regarding the optimal duration of postoperative doses, particularly in TKJR surgery, recommending that, if postoperative doses are administered, prophylaxis should not continue beyond 24 hours (Supplementary Table S1 online).12 We performed an in-depth analysis of the Surgical NAPS orthopedic procedure data subset to provide insight into potential variation across the subcategories and inform clinicians about current SAP prescribing practices and areas for improvement.
In this study, we aimed to describe SAP prescribing practices for orthopedic surgical procedures in Australian hospitals. Secondary aims included assessing SAP appropriateness after accounting for a range of hospital, surgical, and patient factors.
Methods
The key methods adopted for this research have been described previously.Reference Ierano, Thursky and Marshall10 The Surgical NAPS online auditing platform facilitates multicenter, national quality improvement research by collecting a range of data across procedural and postprocedural settings.
Survey metrics
We defined 3 categories of antimicrobial prescriptions for each surgical episode:
procedural, postprocedural, and existing (definitions are outlined in Supplementary Table S2 online). Appropriateness was assessed by trained auditors (ie, pharmacists, nurses and infectious diseases physicians) at the surgical episode level and by each dose and/or prescription. Appropriateness was assessed per dose and/or prescription as a composite measure based on antibiotic choice, timing of administration, and duration by applying the standardized Appropriateness Assessment Guide (Supplementary Fig. S2 online).4,Reference Ierano, Thursky and Marshall10 The survey captures patient demographics (eg, age and gender), clinical information (eg, allergy status, antimicrobial choice, timing, and duration) and procedure-related factors (eg, surgical procedure). The list of surgical procedures and groups was developed from the Royal Australasian College of Surgeons’ morbidity audit and log book tool procedure list (Supplementary Fig. S2 online).
Data collection
The Surgical NAPS was administered as a voluntary survey in both public and private hospitals during any time in the year. Hospitals could participate multiple times over the 3-year auditing period (2016–2019). The updated Therapeutic Guidelines: Antibiotic version 1612 were made available online on April 15, 2019. All procedures from April 18, 2016, through April 15, 2019, were included to focus solely on assessments based on the previous version 1513 or locally endorsed guidelines. Data were collected according to the standardized methodology4,Reference Ierano, Thursky and Marshall10 and were entered via the Surgical NAPS online portal.
Inclusion and exclusion criteria
Surgical episodes with an orthopedic procedure documented as the main procedure were included. In this study, we examined SAP quality; therefore, we excluded existing antimicrobials and postprocedural prescriptions for treatment of infection or with a nonassessable indication. Procedural doses and postprocedural prescriptions that had a ‘not assessable’ appropriateness were also excluded.
Surgical NAPS data collection and analysis were approved by Melbourne Health Human Research and Ethics Committee (approval no. QA2013066).
Statistical analysis
An initial subgroup analysis compared the crude appropriateness of prescriptions when antimicrobials were and were not prescribed for both procedural and postprocedural SAP. Prescription data were stratified into ‘procedural’ and ‘postprocedural’ surgical prophylaxes. Logistic regression models were used to identify hospital, patient, and surgical factors associated with the appropriateness of prescribed doses. For univariate and multivariable analyses, exclusion of the variable was were required if data were missing, were very low in number, and/or were categorized as ‘unknown’ or ‘not assessable.’ The 5 most frequently prescribed antimicrobials accounted for >90% of the data, and the remaining antimicrobials were classified as ‘other.’
Model fitting was initiated with the maximal model including the following factors: peer group, gender, age, allergies, ASA score, surgery number for admission, elective or emergency, trauma, removal or insertion of prosthetic material, wound category, orthopedic procedure group, and antimicrobial. Model selection was performed using likelihood ratio tests, and model fit was assessed using residual plots and goodness-of-fit measures (ie, the C statistic). Mixed-effects logistic models, fit with unique hospital identifiers as random intercepts, provided the best fit to the data and were selected. Two-tailed tests were conducted, and P < .05 was considered statistically significant.
In estimated marginal means analyses, we calculated the mean (% appropriateness) for each variable that was adjusted for the other model variables. This mean is reported as the adjusted appropriateness with 95% CI.
Subgroup analyses were performed for 3 of the orthopedic procedure groups: knees, hips, and open reduction and internal fixations. Procedural and postprocedural data were analyzed separately for each group. The aforementioned best fit model was used to calculate adjusted appropriateness. Our statistical analysis was conducted with Stata version 14.1 statistical software (StataCorp, College Station, TX).
Results
Overall, 140 of 156 hospitals (89.7%) participating in the surgical NAPS survey contributed orthopedic SAP data, representing 20.2% of Australian hospitals with the capacity to perform elective procedures (256 public and 437 private hospitals).14–17 The studied dataset in terms of surgical episodes, procedural doses and postprocedural prescriptions is shown in Figure 1. Orthopedic procedure groups accounted for 4,032 of all surgical episodes (22.0%), inclusive of 8,254 antimicrobial doses and prescriptions in the Surgical NAPS dataset. The median age of patients across these orthopedic surgical episodes was 65 years (range, 0–100). There were similar proportions of males and females (49.9% and 49.1%, respectively).
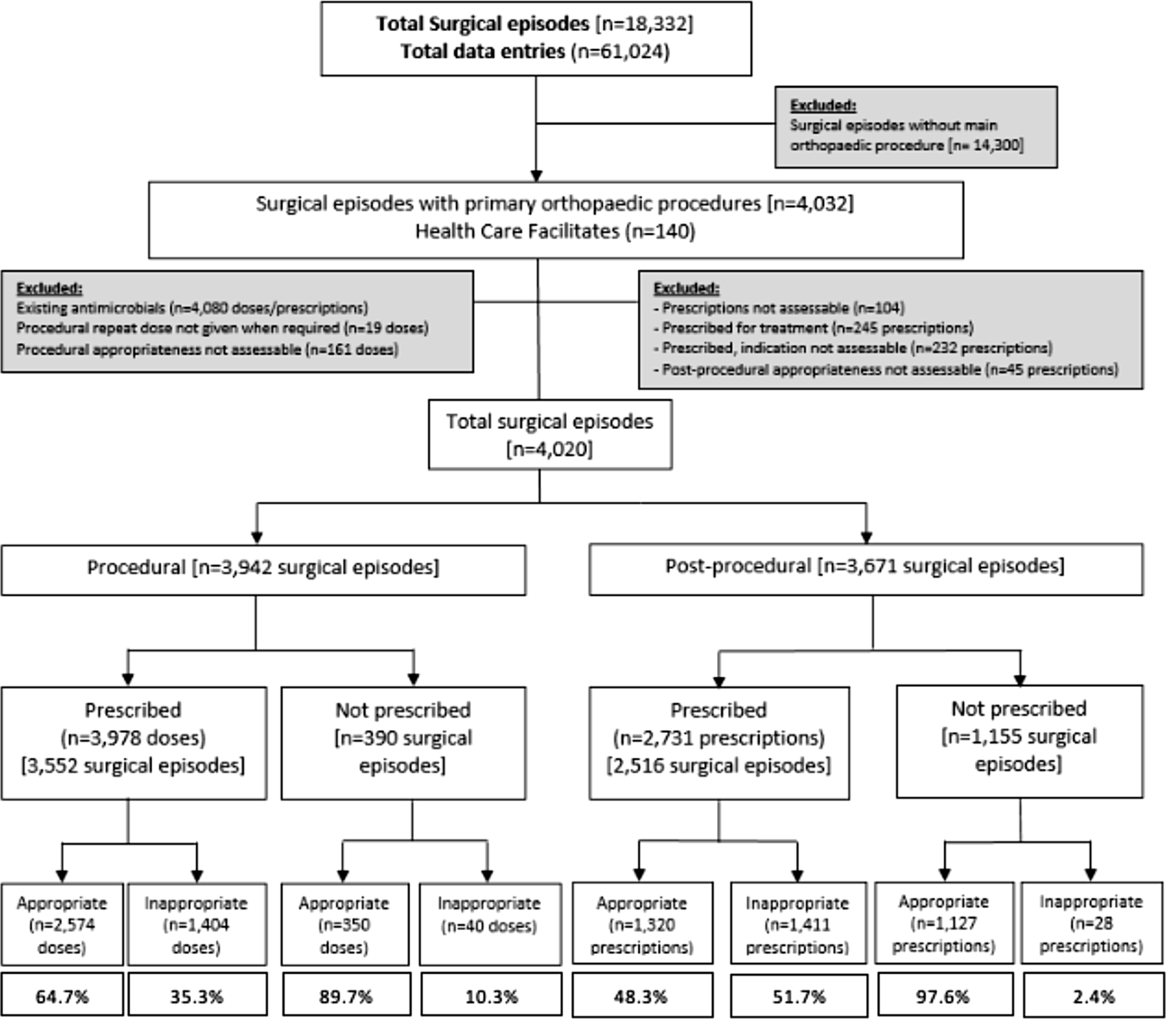
Fig. 1. Audited surgical procedures: study inclusion and exclusion criteria.
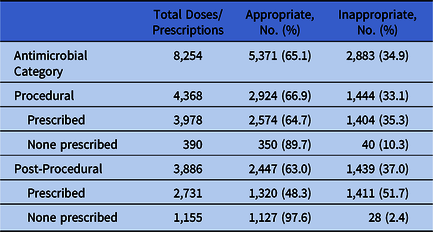
Comparatively, the postprocedural data subset (n = 3,886) had a higher proportion of antimicrobials not prescribed (n = 1,155; 29.7%). The overall appropriateness for prescribed procedural doses (n = 3,978) was 64.7%, and this statistic was lower for prescribed postprocedural doses (n = 2,731; 48.3%). When antimicrobials were not prescribed, appropriateness was much higher for procedural and postprocedural prescriptions (n = 350; 89.7% and n = 1,127; 97.8%, respectively) (Table 1).
Table 1. Comparison of Crude Appropriateness for Prescribed and Nonprescribed Surgical Antimicrobial Prophylaxis
Procedural prescriptions
Procedural prescriptions demonstrated a crude appropriateness of 64.7% (Table 1). Supplementary Table S3 (online) describes the crude and adjusted appropriateness values for all the variables included in the study.
Multivariable analysis revealed the following variables to be significantly associated with increased appropriateness of procedural SAP; peer group–private acute group C hospitals (odds ratio [OR], 3.43; 95% CI, 1.27–9.26; P = .015); 20–39 year-old age group (OR, 1.55; 95% CI, 1.08–2.23; P = .016); and procedures involving removal or insertion of prosthetic material (OR, 2.09; 95% CI, 1.63–2.66; P < .005) (Table S3). The following orthopedic procedure groups were significantly associated with a decrease in procedural SAP appropriateness: knee (OR, 0.26; 95% CI, 0.17–0.41; P < .005), shoulder (OR, 0.49; 95% CI, 0.32–0.74; P = .001), foot and ankle (OR, 0.30; 95% CI, 0.18–0.49; P < .005), hand (OR, 0.32; 95% CI, 0.15–0.69; P = .004), and other (OR, 0.30; 95% CI, 0.19–0.47; P < .005) surgeries. Antimicrobial agents were also associated with a decreased appropriateness including gentamicin (OR, 0.02; 95% CI, 0.01–0.04; P < .005), vancomycin (OR, 0.09; 95% CI, 0.05–0.14; P < .005), and clindamycin (OR, 0.05; 95% CI, 0.02–0.13; P < .005) (Supplementary Table S3 online).
The adjusted appropriateness for all assessable orthopedic procedural doses per orthopedic procedure group is shown in Figure 2. The adjusted appropriateness for each orthopedic procedure group was low, ranging from 54.1% (knee surgery; 95% CI, 46.9–61.4) to 74.1% (TKJR; 74.1%; 95% CI, 69.5%–78.7%). Cefazolin was the most commonly prescribed antimicrobial (86.3% of all procedural doses) and was associated with the highest adjusted appropriateness (73.6%; 95% CI, 69.2%–78.1%). Of the remaining antimicrobials (13.7%), gentamicin was the next most commonly prescribed with 5.2% of procedural doses. The adjusted appropriateness for gentamicin was the lowest of the 5 most frequently prescribed antimicrobials (12.4%; 95% CI, 6.1%–18.7%) (Supplementary Table S3 online).

Fig. 2. Adjusted appropriateness of orthopedic procedural doses per orthopedic procedure groups (%). N = 3,978 assessable orthopedic procedural doses. *Knee surgery excluding total knee joint replacements (eg, knee arthroscopy). **Other surgical procedures included the following subcategories: ‘other,’ ‘soft-tissue surgery,’ ‘sacrococcygeal tumor excision,’ and ‘osteomyelitis (removal of implants/joint washout).’
Subgroup analyses of adjusted appropriateness for specific orthopedic procedures (knee, hip and open reduction internal fracture procedures) were performed (Fig. 3 and Supplementary Tables S5, S7, and S9 online). Knee procedures and diagnostic and therapeutic knee arthroscopies had the lowest rates of adjusted appropriateness: 36.7% and 43.6%, respectively.

Fig. 3. Comparison of procedural and postprocedural adjusted appropriateness across orthopedic surgical procedure subanalyses. aThe model was adjusted for the following variables: peer group, gender, age, allergies, ASA score, surgery admission number, elective or emergency classification, presence of trauma, presence, removal or insertion of prosthetic material, wound category, surgical procedure subcategories and top 5 antimicrobials prescribed per overall data. bProcedural knee subanalysis, model C statistic = 0.8765. cPostprocedural knee subanalysis, model C statistic = 0.9181. dAdjusted appropriateness not estimable due to low number of prescriptions and/or proportions. eProcedural hip subanalysis, model C statistic = 0.8999. fPostprocedural hip subanalysis, model C statistic = 0.9252. gProcedural ORIF subanalysis, model C statistic = 0.8544. hPostprocedural ORIF subanalysis, model C statistic = 0.8762. iUpper limb includes carpus, clavicle, humerus, metacarpal, phalanx, olecranon, radius, scaphoid, and ulna. jLower limb includes ankle, calcaneus, femur, patella, talus, and tibia.
Revision total hip replacements demonstrated a higher adjusted appropriateness (73.0%), than primary hip replacements (66.5%), and ORIF procedures involving the neck of femur had a lower adjusted appropriateness rate (51.1%) than upper limbs (75.3%) and lower limbs (77.8%). When prosthetic material was present, inserted, or removed, the adjusted appropriateness rate was much lower (35.5%). This finding differs greatly from the protective effect of appropriateness that was demonstrated by the presence of prosthetic material on all orthopedic procedures (Table S3).
Supplementary Table S11 (online) highlights the differing rates of appropriateness across the subset of knee procedures for which the evidence supporting SAP is limited and SAP may be required on the basis of the removal or insertion of prosthetic material. When prosthetic material was not present, overall appropriateness was low (42.7%). Comparatively, when prosthetic material was present, removed or inserted, appropriateness was higher (70.9% overall).
Reasons for inappropriateness
Of the 1,404 inappropriate prescriptions, the leading reason for inappropriateness was the administration of SAP when not required (27.2% of inappropriate prescriptions). Knee surgery (excluding TKJR) was the procedure group with the highest rates of procedural SAP prescribed when not indicated (122 of 168 inappropriate prescriptions, 72.6%).
When procedural SAP was indicated and deemed inappropriate (n = 1,022 doses, n = 1,042 documented reasons), the most common reason for inappropriateness was incorrect timing (50.9%), which was consistent across all orthopedic procedure groups (Table 2).
Table 2. Reasons for Inappropriateness of Procedural Doses per Orthopedic Procedure Group

Note. TKJR, total knee joint replacement.
a Rationale for the reasons for inappropriateness are described Surgical NAPS report.4
b Timing was only assessable for procedural prescriptions.
Postprocedural prescriptions
Postprocedural prescriptions had a crude appropriateness rate of 48.3%. Table S4 shows the crude and adjusted appropriateness values for all the hospital, patient, and surgical variables included in the multivariable model. On multivariable analysis (Supplementary Table S4 online), the following variables were associated with appropriateness of postprocedural antimicrobial prescriptions: peer group–private acute group D hospitals (OR, 14.49; 95% CI, 2.69–78.07; P = .002); trauma (OR, 0.45; 95% CI, 0.24–0.83; P = .010); shoulder surgery (OR, 0.46; 95% CI, 0.26–0.81; P = .008); other surgery (OR, 0.47; 95% CI, 0.25–0.90; P < .024); prescriptions of cefalexin (OR, 0.04; 95% CI, 0.01–0.12; P < .005), vancomycin (OR, 0.19; 95% CI, 0.08–0.46; P < .005) and gentamicin (OR, 0.10; 95% CI, 0.03–0.33; P < .005).
The adjusted appropriateness for all assessable postprocedural prescriptions for each orthopedic procedure group category are shown in Figure 4. The adjusted appropriateness for each procedure groups ranged from hand surgery (40.7%; 95% CI, 24.3–57.0) to fractures closed reduction (68.7%; 95% CI, 38.9–95.6).

Fig. 4. Adjusted appropriateness of orthopedic postprocedural prescriptions per orthopaedic procedure groups (%); n = 2,731 assessable orthopedic postprocedural prescriptions. *Knee surgery excluding total knee joint replacements (eg, knee arthroscopy). **Other surgical procedures included the following subcategories: ‘other’, ‘soft-tissue surgery,’ ’Sacrococcygeal tumor excision,’ and ‘osteomyelitis (removal of implants/joint washout).’
Cefazolin was the most commonly prescribed antimicrobial, at 85.9% of all postprocedural doses, and it had the highest rate of adjusted appropriateness (55.2%; 95% CI, 48.4–61.9). Cefalexin was the second most commonly prescribed antimicrobial (4.2%) and demonstrated the lowest rate of adjusted appropriateness (17.2%; 95% CI, 6.6%–27.8%) of the 5 most frequently prescribed antimicrobials (Supplementary Table S4 online). Subgroup analyses of adjusted appropriateness for knee, hip, and open-reduction internal-fracture procedures were performed (Fig. 3 and Supplementary Tables S6, S8, and S10 online). For knee procedures, osteotomy procedures demonstrated the lowest rates of adjusted appropriateness (50.6%). Primary TKJRs had a lower adjusted appropriateness than revisions (51.8% vs 63.0%). Primary THJRs demonstrated a higher adjusted appropriateness (52.6%) than revisions (51.9%). When prosthesis was involved in neck of femur ORIFs, the adjusted appropriateness was lower (40.1%) than with no prosthesis (44.6%).
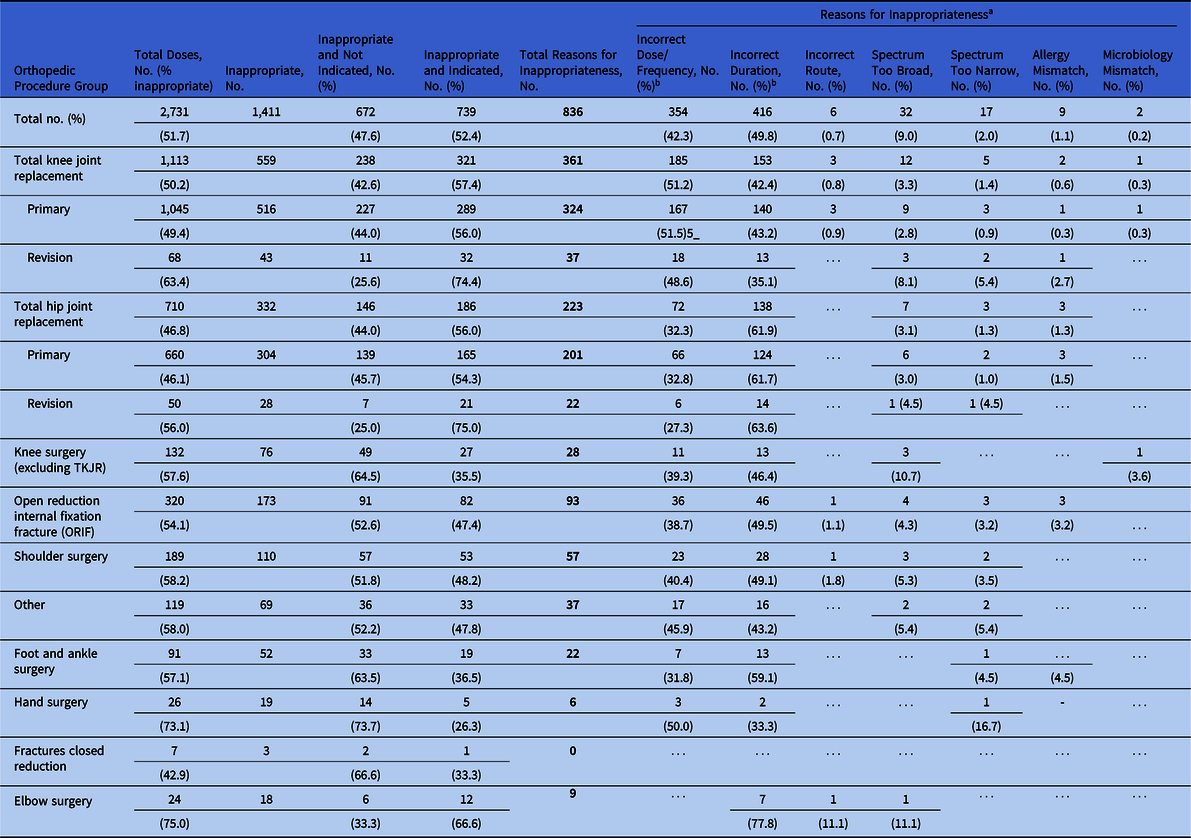
Reasons for inappropriateness
Of the 1,411 inappropriate prescriptions, 47.6% were inappropriate because postprocedural SAP was not indicated (Table 3). The procedure groups with the highest rates of postprocedural SAP prescribed when not indicated were hand surgery (73.7% of 19 inappropriate prescriptions) and foot and ankle surgery (63.5% of 52 inappropriate prescriptions) (Table 3). When postprocedural SAP was indicated and was deemed inappropriate (n = 739 prescriptions, n = 836 documented reasons), the most common reason for inappropriateness was incorrect duration (49.8%), followed by incorrect dose and/or frequency (42.3%); this finding was consistent across all orthopedic procedure groups (Table 3).
Table 3. Reasons for Inappropriateness of Postprocedural Prescriptions per Orthopedic Procedure Group
Note. TKJR, total knee joint replacement.
a Rationale for the reasons for inappropriateness are described Surgical NAPS report.4
b Duration and frequency were only assessable for postprocedural prescriptions.
Discussion
To our knowledge, our study is the first to examine appropriateness of procedural and postprocedural SAP prescriptions across a range of orthopedic procedures in Australian hospitals. Our analysis has identified suboptimal rates of appropriate SAP prescriptions when accounting for a range of hospital, patient, and surgical factors. Detailed analyses and comparison of SAP prescription appropriateness across specialty surgical procedures subgroups facilitated meaningful assessments for targeted stakeholder groups, such as orthopedic surgeons.
Inappropriate and guideline noncompliant SAP for orthopedic procedures been reported consistently in Australian4,6,Reference Ierano, Thursky and Marshall10,Reference Bull, Worth and Spelman18 and international literature.Reference Ou, Jing and Guo7–Reference Pittalis, Ferraro and Piselli9,Reference Khan, Ahmed and Rehman19–Reference Branch-Elliman, Pizer and Dasinger21 Although orthopedic procedures are commonly audited for SAP, the current literature demonstrates a limited number of studies that compare a subset of orthopedic procedures,Reference Khan, Ahmed and Rehman19 as opposed to comparing orthopedic procedures as a whole to other surgical specialties (eg, cardiac and abdominal).Reference Ou, Jing and Guo7,Reference Mousavi, Zamani and Bahrami8,Reference Ierano, Thursky and Marshall10
One driver for the identified variation in practice may be lack of awareness of SAP guidelines, particularly for specific procedures. A questionnaire performed by the Orthopaedic Trauma Association highlighted heterogeneity in opinions regarding guideline value and evidence quality for single- versus multiple-dose SAP for closed long-bone fractures.Reference Gans, Jain and Sirisreetreerux22 The participating surgeons reported low awareness of SAP guidelines; however, they were receptive to changing their practice to single-dose SAP if the change were supported by high-level evidence.Reference Gans, Jain and Sirisreetreerux22 Similar Australian perceptions of the evidence may be reflective of our identified suboptimal adjusted appropriateness for SAP in closed bone fractures (68.2% procedurally and 68.7% post procedurally) (Figs. 2 and 4).
There is limited and conflicting evidence to support SAP for diagnostic and therapeutic shoulder and knee arthroscopyReference Baraza and Leith23–Reference Carney, Heckmann and Mayer25 and hand surgery.Reference Dunn, Fares and Kusnezov26 National and international guidelines do not recommend the use of SAP in routine arthroscopic procedures unless the procedure involves insertion of prosthetic material or avascular tissue.12,13,Reference Bratzler, Dellinger and Olsen27 Our study identified that these procedures had the highest rates of procedural inappropriateness due to administration when not required: shoulder (45.4%), knee (72.6%), and hand surgery 65.4% (Table 3). Therefore, we suggest greater dissemination of specific evidence and guideline recommendations for these procedures; engagement with these niche specialties is required to understand fully the motivating factors for continued prescribing of SAP for these procedures (Fig. 4).
Our analysis revealed that postprocedural administration of SAP when not required accounted for almost half (47.6%) of all inappropriate postprocedural prescriptions. Duration of postprocedural SAP remains controversial, especially for hip and knee arthroplasty. Most guidelines and professional bodies do not recommended SAP after wound closure.Reference Berríos-Torres, Umscheid and Bratzler11–13,Reference Bratzler, Dellinger and Olsen27,Reference Aboltins, Berdal and Casas28 However, the American Association of Hip and Knee Surgeons (AAHKS) argues that recommendations for single-dose SAP are not supported by the available evidence.Reference Yates29 In our surveyed population, incorrect duration and dose and/or frequency were the most common reasons for inappropriateness for postprocedural prescriptions. This finding highlights these components of SAP prescribing as critical areas for quality improvement. The consequences of antibiotic overuse, such as prolonged SAP duration, have been well described in the literature and include lack of SSI reductionReference Branch-Elliman, O’Brien and Strymish30 and patient harms such as antibiotic side effects,Reference Tamma, Avdic and Li31 Clostridioides difficile infections,Reference Branch-Elliman, O’Brien and Strymish30,Reference Tamma, Avdic and Li31 acute kidney injury,Reference Branch-Elliman, O’Brien and Strymish30 and contribution to antimicrobial resistance.Reference Branch-Elliman, O’Brien and Strymish30
Qualitative research in AustraliaReference Broom and Broom32,Reference Ierano, Thursky and Peel33 and the United KingdomReference Charani, Tarrant and Moorthy34 has highlighted potential influences on SAP prescribing culture. The fear of causing patient harm, such as surgical site infections,Reference Broom and Broom32,Reference Ierano, Thursky and Peel33 and litigation claims for malpracticeReference Broom and Broom32,Reference Ierano, Thursky and Peel33 have been identified as drivers for overuse of SAP. Further education is required to communicate the evidence that antimicrobial overuse may also cause significant patient harm.
A multicenter national retrospective cohort study of the US Veterans’ Affairs healthcare system with 79,058 patientsReference Branch-Elliman, O’Brien and Strymish30 demonstrated that the adjusted odds ratio (aOR) for SSIs in orthopedic procedures increased when SAP was administered for >24 hours: 24–48 hours (aOR, 1.11; 95% CI, 0.82–1.51); 48–72 hours (aOR, 2.04; 95% CI, 1.00–4.16); and >72 hours (aOR, 1.63; 95% CI, 0.22–12.07).
A novel retrospective study of 20,382 primary TKJRs and THJRs compared single-dose (n = 4,523) SAP to multiple doses: procedural and postprocedural SAP (n = 16,159).Reference Tan, Shohat and Rondon35 No difference in the PJI rate was detected at 1 year between single- and multiple-dose SAP: univariate analysis (aOR, 0.674; P = .064); multivariate analysis (aOR, 0.755; P = .205); and propensity score matched analysis (aOR, 0.746; P = .277). Specifically, patients who received single-dose cefazolin were more likely to have a lower rate of PJI than those who received multiple doses (over 24 hours) (P = .054).Reference Tan, Shohat and Rondon35
Most recently, a systematic review with meta-analysis of 52 RCTs (n = 19,273 participants across multiple surgical procedure types) demonstrated that no significant benefit (SSI reduction) accrued from prolonging SAP (in comparison to no postoperative doses), with a pooled RR of 0.89 (95% CI, 0.79–1.00).Reference De Jonge, Boldingh and Solomkin36 Multiple recent studies advocate for a well-powered, randomized, prospective trial comparing infection outcomes using single- and multiple-dose SAP regimens for TKJR.Reference Branch-Elliman, O’Brien and Strymish30,Reference Tan, Shohat and Rondon35,Reference Siddiqi, Forte and Docter37,Reference Thornley, Evaniew and Riediger38 Importantly, Duke University and the AAHKS are conducting a multicenter clinical trial (estimated n = 8,000) comparing single dose and prolonged duration (24 hours) of SAP for elective primary TKJR and whether this significantly reduces the incidence of prosthetic joint infections (ClinicalTrials.gov Identifier: NCT03283878; estimated completion date October 2020).
This research has a number of limitations. Although the audit captured ~20% of Australian hospitals performing elective procedures, reasons for nonparticipation are not known. This factor may limit the generalizability of our results to other Australian and international centers. A mixed-effects regression model accounted for the intrahospital correlations; however, the effects of an unbalanced survey design may persist. The variation in ‘appropriate assessments’ is probably due to multiple auditors. However, a validation study4 comparing assessments between local auditors and the NAPS clinical support team demonstrated a low rate of disagreement (6.7%).
Our large, national audit demonstrated low rates of SAP appropriateness across orthopedic procedures. Our analysis identifies niche areas for orthopedic SAP optimization, including procedures where procedural SAP is prescribed when not required and when multiple postprocedural doses are given when not indicated. These data provide meaningful metrics to support the development of quality improvement programs in orthopedic surgery.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ice.2020.320
Acknowledgments
We thank the National Antimicrobial Prescribing Survey (NAPS) Support team for their ongoing assistance with Surgical NAPS data collation and website management; Ms Caroline Chen, Ms Robyn Ingram, A/Prof Noleen Bennett, Ms Xin Fang and Mr Ron Cheah.
We thank Dr Arjun Rajkhowa, NCAS Centre Manager for his administrative support with this manuscript.
Financial support
Surgical NAPS is funded by the Australian Commission on Safety and Quality in Health Care as part of the National Antimicrobial Use and Resistance in Australia Surveillance System; the Australian Government Department of Health, the National Centre for Antimicrobial Stewardship and Melbourne Health.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.