Introduction
Racial and ethnic inequities in health outcomes are well-documented. 1 Although patient-related risk factors may influence out-of-hospital events and disease-related outcomes, the care provided to the patient within the hospital is expected to be consistent, regardless of the patient’s racial and ethnic background. Consequently, the incidence of healthcare-associated conditions (including infections) should also be equally distributed across racial and ethnic groups. Reference Lyren, Haines and Fanta2 However, numerous reports in the literature have shown that this is not the case, and disparities in complications associated with healthcare delivery have been observed. Reference Shen, Cochran and Mazurenko3,Reference Willer, Tobias, Suttle, Nafiu and Mpody4
Shen et al., in an analysis of National Inpatient Sample data, found a higher incidence of pressure ulcers among Black and Asian/Pacific Islander individuals, as well as those with public insurance, compared to White individuals and those with private insurance. Reference Shen, Cochran and Mazurenko3 Their analysis, however, was not adjusted for comorbidities and disease states. In a study of children from the Pediatric Health Information System database, Willer et al. Reference Willer, Tobias, Suttle, Nafiu and Mpody4 found that the unadjusted relative risk of central line-associated blood-stream infections (CLABSI) was higher for Black children and Hispanic children. However, this analysis did not adjust for line dwell time, a significant exposure risk. Additionally, a higher rate of preventable adverse events in hospitalized Latino children Reference Stockwell, Landrigan and Toomey5 and in patients with limited English proficiency has also been reported. Reference Khan, Yin and Brach6 Most of these studies have the limitation of using databases not primarily designed to address racial disparities, along with the limitations inherent in administrative data, such as the inability to account for exposure risk (central line days).
While all patients with central lines are at risk of developing infections, the risk is not uniformly distributed across all disease states. Specific populations such as those admitted to the Intensive Care units, Reference Moriyama, Ando and Kotani7 Oncology patients, Reference Martinez, Santo and Godinho8 and the utilization of the central line itself (for example, for administration of Total Parental Nutrition [TPN] Reference Lafuente Cabrero, Terradas Robledo and Civit Cuñado9 ), have been shown to have a higher risk of CLABSI. Moreover, these disease states and utilization may not be consistently spread across different racial and ethnic categories, thus exposing them to different risks of CLABSI. 10
This retrospective chart review was designed to compare risk-adjusted central line-associated bloodstream infection rates (adjusted for exposure per 1,000 central line days) based on patients’ race and ethnicity. We hypothesized that even after adjusting for patient-level risk factors, differences in central line infection rates exist among various racial and ethnic categories. The secondary objective was to compare the outcomes (hospital length of stay, mortality) of patients who developed CLABSI vs those who did not.
Methods
This multi-institutional retrospective study was conducted on patients of all age groups admitted to any hospital within the OSF HealthCare network between January 1st, 2018, and June 30th, 2023. OSF Healthcare comprises 15 inpatient facilities in Illinois and Michigan, with 2,134 licensed beds and over 80,000 admissions/year, including over 7000 pediatric admissions. 11
Only patients with a central line insertion and removal documented during the same hospitalization were included in the study. Patients with pre-existing central lines and those with an indwelling central line at discharge were excluded. Tunneled central lines were also excluded. To reduce dependency resulting from repeated measurements of the same patient, the data were limited to the first admission of each patient during the timeframe. Separate lines within the same encounter were grouped, and the total CLABSI count and catheter days for the encounter were calculated. The Institutional Review Board of the University of Illinois College of Medicine at Peoria reviewed and approved the study. The need for informed consent and HIPAA authorization was waived due to the study’s retrospective nature.
The primary outcome variable was catheter-associated central line infection, identified based on reporting to the Centers for Disease Control’s National Healthcare Safety Network as CLABSI. 12 Central line days were extracted based on the documented central line insertion and removal dates in the electronic health record (EHR). Patients’ self-reported race and ethnicity, as entered in the EHR, were also extracted. Race and ethnicity categories were defined according to the Office of Management and Budget’s standard criteria. 13 The raw data from the EHR included 17 race and eight ethnic categories (Summary information of all race and ethnic distribution available in Supplemental Digital Content [SDC] 1). For statistical analysis, the racial and ethnic categories were combined into Hispanic, non-Hispanic White, non-Hispanic Black, and non-Hispanic others for analysis, as previously reported. 14 Other variables extracted from the EHR included patient age (in years), insurance status (10 categories coded as public/private, SDC 2), sex (male/female, as assigned at birth), primary language (48 categories, dichotomized as English and non-English, SDC 3), and diagnosis. Specific diagnostic categories known to be associated with CLABSIs, such as diabetes, dialysis, TPN, antineoplastic therapy, blood product administration, immune deficiency, severe neutropenia, and cancer, were identified from the EMR based on pre-specified criteria (SDC 4) and coded as yes/no. Other outcome variables extracted included ICU admission, intubation during admission, hospital length of stay, ICU length of stay, and mortality.
The primary statistical analysis involved a univariate comparison of the CLABSI rate (per 1,000 central line days) based on patients’ race and ethnicity. Poisson regression was used to model the CLABSI rate per catheter day, using the count of CLABSIs associated with the patient and including the log of catheter days for an encounter as an offset. This approach controlled for potential confounding variables. Confounding variables were selected based on potential relations with race/ethnicity and the risk of CLABSI. The causal structure for the regression model is shown in Figure 1. Unmeasured confounders, such as the severity of illness and economic disparities, were blocked using surrogate variables of ICU admission (yes/no) and insurance status (public/private). Reference Williams, Bach, Matthiesen, Henriksen and Gagliardi16 The dispersion ratio of 0.90 from a Poisson regression indicated under dispersion, violating the assumption that the mean and variance are equal. Therefore, a generalized Poisson regression, which is appropriate for both under- and overdispersion, was used. The ratio of observed to predicted zero counts was used to check for zero-inflation and was found to be 1, indicating that the model was not zero-inflated. A random intercept for the hospital was also included to account for hospital-level clustering. Post hoc subgroup analysis was also performed separately for adult and pediatric patients. For pediatric patients, due to the small sample size, only an unadjusted comparison of CLABSI rates (exact rate ratio test with Holm-Bonferroni adjustment for multiple comparisons) between the racial/ethnic groups was made. All statistical analysis was performed using the open statistical program R 17 and JMP Pro V17.0 (SAS Inc, Cary, NC).

Figure 1. Causal Directed Acyclic Graph. Reference Textor, Van der Zander, Gilthorpe, Liśkiewicz and Ellison15 Each line on the graph represents a single directional flow from one node to the other. In this model, chronic illness, central line utilization, economic disparities, language, age distribution, and severity of illness are expected to be common causes (association with) of race and ethnicity and central line-associated blood-stream infection. White nodes (circles) represent conditioned/blocked path (included in the regression model). While pink nodes represent unblocked path. Variables that cannot be accurately measured are blocked by surrogate (proxy variables). They do not completely block the path, so possibility of bias remains https://dagitty.net/dags.html?id=N59gtFf2.
Results
A total of 31,814 central lines were placed in 23,133 unique patients across 26,686 hospital admissions. The data were limited to the first admission and grouped by MRN for analysis. A total of 27,674 central lines were included, accounting for 245,889 catheter days. There were 263 CLABSIs reported, resulting in an overall CLABSI rate of 1.070 per 1000 central line days. The most common line type was CVC (12,469 [45.1%]), followed by Peripherally Inserted Central Catheter (PICC) (12,308 [44.5%]), dialysis catheters (1937 [7.0%]), and Umbilical Vein (UV) catheters (960 [3.5%]). The median age of the study population was 64 years (IQR 49.9–74.4), with 8% of patients under 18 years of age. A large proportion of the patients were non-Hispanic White (17,619 [76.2%]), followed by non-Hispanic Black (3967 [17.1%]), and Hispanic (1006 [4.3%]). The remaining racial/ethnic groups were classified as other/unknown (541 [2.3%]). Up to 77% (17,872/23,133) of patients had public health insurance, and 62% (14,437/23,133) required ICU admission during hospitalization. The respective proportions of various comorbidities and line utilizations are provided in Table 1.
Table 1. Patient demographic and clinical characteristics. Overall N = 23, 133

a Missing 12 (0.1%).
Unadjusted CLABSI rate comparisons
Table 2 presents the number of lines, CLABSI counts, catheter days, and CLABSI rates based on various demographic variables. The most notable difference in CLABSI rates was observed between adult and pediatric populations. The CLABSI rate for adult patients was 0.931 per 1000 catheter days, compared to 1.926 per 1000 catheter days for children (P < .001). Patients admitted to the ICU also had a higher CLABSI rate at 1.351 per 1000 catheter days compared to patients admitted only to general floors (0.427 per 1000 catheter days), P < .001. Among the various racial/ethnic groups, the highest CLABSI rate was observed in the Hispanic population (1.875 per 1000 catheter days), while the lowest rate was seen in non-Hispanic Whites (0.971 per 1000 catheter days). The difference between CLABSI rates of Hispanic vs non-Hispanic White population was significant at P = .018, but not for non-Hispanic Black and non-Hispanic White. No difference in CLABSI rate was observed based on insurance class, language, or sex.
Table 2. Central line-associated blood-stream infection (CLABSI) rates based on different demographic categories
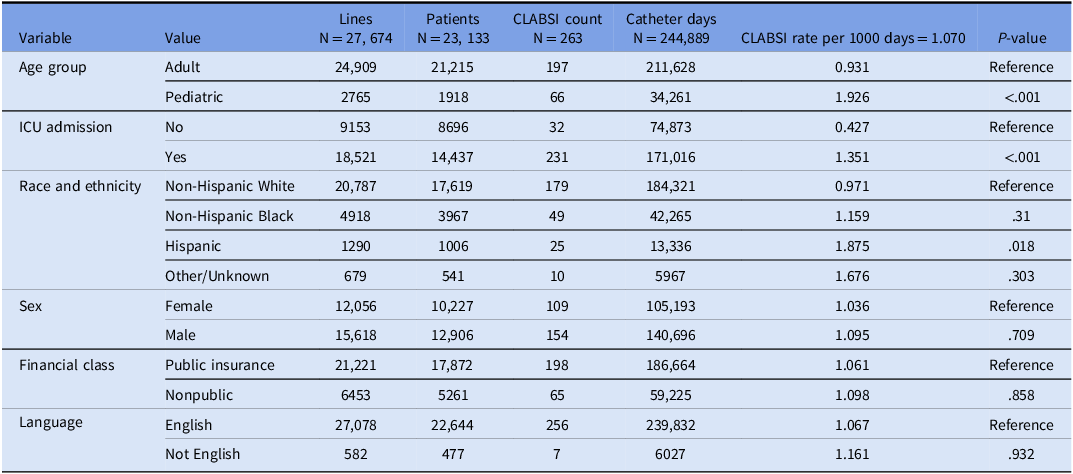
The other category included American Indian or Alaska native (47), Asian (117), Asian Indian (8), Chinese (2), Filipino (3), Japanese (1), Korean (1), Native Hawaiian (2), Missing (11), Other (180), Other Asian (6), Other Pacific Islander (7). Patient refused (12), Unknown (141), Vietnamese (3).
Table 3 provides similar information based on various diagnostic categories and line usage. Among the six diagnostic cohorts tested, a significant difference was observed within CLABSI rates of patients with cancer (1.572 vs 1.007/1000 catheter days, P = .013), immunodeficiency (3.328 vs 0.993/1000 catheter days, P < .001) and severe neutropenia (4.563 vs 0.977/1000 catheter days, P < .001. Patients with diabetes had lower rates of CLABSI compared to patients who did not have diabetes (0.745 vs 1.179/1000 catheter days, P = .004). Antineoplastic medications, blood product administration during hospitalization, and order of TPN were associated with higher CLABSI rates compared to those who did not receive these treatments.
Table 3. Central line-associated blood-stream infection (CLABSI) rates based on various diagnostic categories and central line use

Adjusted results from the regression model
Generalized Poisson regression for the count of CLABSI per patient showed that Hispanic patients had a higher CLABSI rate per 1000 catheter days compared to non-Hispanic White patients after controlling for all included potentially confounding variables (incident rate ratio [IRR] 1.89, 95% CI 1.15–3.10, P = .013). There was no significant difference in the IRR between non-Hispanic Black and non-Hispanic White patients. Holding all other variables constant at their reference values or means, and the offset of log catheter days at the mean, the adjusted CLABSI rates per 1000 catheter days were expected to be 2.01 (95% CI 1.23–3.27) for non-Hispanic Whites, 2.08 (95% CI 1.19–3.62) for non-Hispanic Blacks, and 3.79 (95% CI 1.97–7.3) for Hispanic patients. Full regression results are presented in Table 4. Subgroup analysis limited to adult patients only (n = 21,203) also showed higher IRR for Hispanic patients, but the difference did not reach statistical significance (IRR 1.49, 95% CI 0.75–2.95, P = .25) (SDC 5). For pediatric patients, the unadjusted CLABSI rate for Hispanic patients was higher than non-Hispanic White (3.35/1000 line days vs 1.46/1000 line days, P = .032). However, after the Holm-Bonferroni adjustment, the P-value was not significant at .095 (SDC 6).
Table 4. Regression results for central line-associated blood-stream infection rate per 1000 central-line days

N location = 15. Observations = 23, 121. TPN Total Parenteral Nutrition, ICU Intensive Care Unit.
Unadjusted comparison of outcomes
Patients who developed CLABSI had significantly worse outcomes than patients who did not develop CLABSI. Patients who developed CLABSI stayed in the hospital for a significantly longer period, with the median hospital length of stay of 30 (IQR 17, 55.2) compared to 9 (IQR 5, 16) of patients who did not develop CLABSI, P < .001. Among patients who required ICU admission, the median length of stay of patients who developed CLABSI was 18.1 (IQR 10.0, 48.9, n = 188) compared to 4.1 (1.9, 9.3, n = 14,249) days for patients who did not develop CLABSI. Of 23,133 patients, 4188 died during the hospital encounter (18.1%). The mortality rate was 35.5% for those with CLABSI (78/220) compared to 18% (4110/22,913) for patients without CLABSI. (SDC 7)
Discussion
In this multi-institutional study of more than 27,000 central lines from 15 hospitals, we demonstrated that after adjusting for potential diagnostic and line usage-related risk factors, there is no difference in CLABSI rates for NHB and NHW, but the CLABSI rate for the Hispanic population is higher. While prior studies have identified disparities based on race and ethnicity, our study adds to the literature by providing patient-level, risk- and exposure-adjusted analyses.
Our study design is similar to a recently published manuscript by Gottlieb et al. Reference Gottlieb, Prakash-Asrani, Dube, Wiley, Licitra and Fridkin18 Similar to our data, they did not demonstrate any difference in the risk-adjusted CLABSI rates between NHB and NHW. While Hispanic patients were included in their initial analysis, their final adjusted Cox regression model only compared NHB and NHW patients, limiting direct comparison with our results. Higher CLABSI risk in the Hispanic population has, however, been described in other studies. Anila Bakullari et al. Reference Bakullari, Metersky and Wang19 calculated hospital-associated infection (HAI) rates in a randomly selected sample of 79,000 Medicare patients from the Medicare Patient Safety Monitoring System between 2009 and 2011. They reported age-, gender-, and comorbidity-adjusted odds ratios for HAI that were statistically significantly higher for Hispanic and Asian populations. Although this study had a large sample size, it captured relatively few CLABSIs (76 out of 5800 patients with central lines), limiting its applicability to CLABSI risk. A similar, more recent study of children from the Pediatric Health Information Systems database found that the relative risk of CLABSI was 1.274 for Black and 1.164 for Hispanic children compared to White children. The variables adjusted for included age, sex, median household income by ZIP code, central line type, and the presence of complex chronic conditions. Reference Willer, Tobias, Suttle, Nafiu and Mpody4 However, this analysis also did not adjust for exposure (line days), which somewhat limited its validity. This limitation was addressed by a group at Solutions for Patient Safety (SPS). In an analysis from 25 US children’s hospitals, they showed that CLABSI rates for Hispanic patients were three standard deviations above the network average. Similar to our study, no difference was observed in CLABSI rates for non-Hispanic Black patients. Due to the de-identified nature of the SPS data, patient-level risk factors could not be adjusted in this study. Reference Lyren, Haines and Fanta2 In our study, the post hoc subgroup analysis, limited to adult or pediatric patients, showed higher CLABSI rates in Hispanic patients, but the effect was smaller and did not reach statistical significance. This may be related to the inherently reduced sample size for the subgroups, and our study may not be powered to detect the difference in subpopulations. It is also possible that the effect is concentrated in particular portions of the data, which may be driving the overall observed differences. Further adequately powered studies on subpopulations may provide additional insights into the possible sources of the disparity.
While not a primary objective of this study, the unadjusted worse outcomes of patients with CLABSI observed in our study are in concordance with multiple prior reports. Reference Ziegler, Pellegrini and Safdar20,Reference Stevens, Geiger, Concannon, Nelson, Brown and Dumyati21 With the demonstrated ethnic disparities in the risk of CLABSI, the association of poor outcomes in patients who develop CLABSI brings to focus the implications of this disparity in influencing the overall health outcome disparities in hospitalized patients in the United States. Obesity, immune deficiency, and use of TPN and blood products were other factors independently associated with CLABSI in our regression model. Many of them have also been identified as risk factors for CLABSI in prior reports, including a recent meta-analysis. Reference Lafuente Cabrero, Terradas Robledo and Civit Cuñado9
Although our study was not explicitly designed to address the potential causes of the observed disparities, the residual differences in CLABSI after adjusting for baseline characteristics and line utilizations related risk may suggest gaps in the processes of care. Potential root causes for racial disparity may include: a) barriers to access due to social and economic challenges leading to delayed presentation and consequently higher disease severity, which may not be completely adjusted; b) healthcare system barriers such as language and cultural differences between providers and patients. Previous research has shown a correlation between cultural and linguistic barriers in the incidence of CLABSI. Reference Di Gangi, Pini and Baccelli22 It is possible that when patients are well informed about their central line care, they can actively participate in infection prevention, which may lead to earlier recognition of signs and symptoms and shared decision-making. Although language (ie, English as a non-primary language) was included in our model, this variable may not have been captured accurately, as patients may hesitate to report English proficiency to their healthcare providers; c) implicit bias among healthcare providers, and d) variations in adherence to the CLABSI prevention protocol. Higher compliance with CLABSI prevention bundles have been shown to have a modest but significant correlation with lower CLABSI rates. Reference Tripathi, McGarvey and Lee23 Differences in bundle compliance across patients from different ethnic or socioeconomic backgrounds have not been explored in the literature and may yield further insights into the factors behind the disparities. Successful infection prevention control strategies are likely to be those that align with the cultural contexts in which they are implemented Reference Borg24 and training in cultural competency for healthcare providers has been shown to improve patient-provider communications. Reference Jongen, McCalman and Bainbridge25 Adapting “care bundles” to accommodate the unique racial and cultural differences of various patient populations and equity focused infection prevention strategies may offer a potential approach to promote improvement. Reference McGrath, Bettinger and Stimpson26
The main limitation of analyses such as ours is unadjusted confounding. While variables such as exposure (line days) can be reliably captured, comorbid diagnoses (eg, diabetes, cancer) rely on accurate data entry in the EHR. Even when comorbidities are captured accurately, most exist on a spectrum, and binary (0/1) adjustments in statistical regression may not fully account for their influence. The severity of illness and socioeconomic status were likely incompletely captured by ICU admission and insurance status, respectively. Additionally, as a social construct, race and ethnicity often overlap, and a large proportion of patients are likely multiracial. While we categorized patients into clear “buckets” for analysis, there may be more heterogeneity in the study population than our data reflects. Although our study included data from 15 hospitals, most were in the Midwest, and the Hispanic Population was underrepresented compared to the overall US population. Small proportion of Hispanic patients can lead to unreliable estimates and may impact robustness of our findings. Additionally, the barriers to access may be less pronounced in regions with a larger representation of Hispanic patients, and further studies in such racially diverse regions are recommended to replicate our findings and for more comprehensive adjustment of confounders. Our analysis was limited to the first admission to maintain the validity of the statistical tests. However, this precludes our ability to identify patients with recurrent CLABSI risk. This may underrepresent the actual burden of infection among high-risk populations.
Conclusion
Hispanic patients are more likely to have hospital-associated CLABSIs compared to non-Hispanic White patients, even after adjusting for measured exposure and patient-level risk factors.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/ice.2025.8
Acknowledgments
We acknowledge Ms. Alaina Mabie from the Division of Research Services, Department of Pediatrics at the University of Illinois College of Medicine at Peoria, for helping obtain regulatory approvals for this study. The authors disclose no financial support for this study and publication and no conflict of interest.
Author contribution
Dr. Tripathi conceived and designed the project. He obtained regulatory approvals and assisted in data extraction, validation, and statistical analysis. Dr. Tripathi also performed the literature search and drafted the final manuscript. Ms. Walters performed all data extraction and validation from the EMR. Mr. McGarvey performed statistical analysis and interpretation. All authors have reviewed and approved the final manuscript as submitted.