Introduction
Obsessive–compulsive disorder (OCD) is a prevalent and disabling condition that determines a significant reduction of the quality of life in affected patients.Reference Robbins, Vaghi and Banca 1 With a lifetime prevalence around 2% to 3%, OCD is frequently under-recognized and its duration of untreated illness was found to range between 4 and 8 years.Reference Vigne, Fortes and Dias 2 The wide variability of symptoms’ presentation heavily influences the diagnostic delay; while most severe forms are easily recognized, the milder or subthreshold presentations are often not detected and treated for many years.Reference Fineberg, Hollander and Pallanti 3 Indeed, subthreshold forms were found to be associated, on one hand, with less severe symptoms but, on the other hand, with an impaired quality of life.Reference de Bruijn, Beun and de Graaf 4 Moreover, comorbidity with other psychiatric disorders, such as anxiety and depressive disorders, often generates diagnostic complexity and suboptimal OCD treatment.Reference Lochner, Fineberg and Zohar 5 It has to be noticed that alexithymia may be present in 30 to 40% of patients with OCD and it has been linked to increased severity and lower insight in OCD patients.Reference De Berardis, Serroni and Marini 6 , Reference De Berardis, Di Natale and Carletti 7 Available literature has already described different treatment strategies based on the severity of the clinical picture; while in full-blown forms of OCD, pharmacological and integrated treatment guidelines are clearly defined, limited therapeutic approaches are present for moderate or subthreshold forms.Reference Janardhan Reddy, Sundar, Narayanaswamy and Math 8 , Reference Karas, Lee and Jimenez-Shahed 9 Full-blown OCD shows chronic/progressive course in the majority of published reports, although a waning and waxing/fluctuant course and an episodic course have also been described.Reference Sharma and Math 10 In this scenery, the growing interest in staging methods in psychiatry may play a relevant role in defining prognosis and treatment of OCD, even in the early stages or in subthreshold forms of the disease.Reference Fineberg, Dell'Osso and Albert 11
Clinical staging is based on the concept that psychiatric illnesses progress over time through consecutive stages, characterized by symptoms of increased intensity—from stage 0 (increased risk, asymptomatic) to stage 4 (severe illness)—and it seeks to define both the disease progression and the differentiation of milder clinical phenomena from more severe presentations.Reference McGorry 12 , Reference Cosci and Fava 13 Potential advantages in the use of staging models are represented by the timing improvement of therapeutic interventions—assessed in relation to their ability to prevent/delay the progression of illness from earlier to later stages—and the promotion of a better therapeutic personalization.Reference Sharma and Math 10 Staging models have been proposed and applied to different mental disorders, such as schizophrenia and psychotic spectrum disorders,Reference Fineberg, Dell'Osso and Albert 11 bipolar disordersReference Cosci and Fava 13 and, more recently, in OCD as well.Reference Storch, De Nadai and Conceição Do Rosário 14 , Reference Fontenelle and Yücel 15 OCD seems to be suitable for the application of staging models, particularly in the early stages of the illness, in light of its early onset and longer duration of untreated illness (DUI), compared to other psychiatric disorders. In a recent report, Fontenelle and coauthorsReference Fontenelle and Yücel 15 proposed a staging model for OCD based on the integration of symptom severity and phases of illness, with special focus on early diagnosis and subthreshold forms. The authors identified four stages and correlated each of these stages with the most appropriate form of intervention, providing a prototype of therapeutic algorithm based on OCD stage. For instance, in healthy individuals (stage 0), characterized by absence of symptoms but in presence of risk factors (family history for OCD, presence of tic disorder), psychotherapy and psychoeducational interventions are indicated as effective when associated to periodical clinical assessment. As regards subthreshold forms (stage I), meditation programs or cognitive behavioral therapy are indicated, along with lifestyle improvement. Patients with greater clinical severity were subdivided according to Yale-Brown Obsessive–Compulsive Scale (Y-BOCS) scores in stage II (Y-BOCS scores between 14 and 34) and stage III (Y-BOCS scores higher than 35). Pharmacological and brain-stimulation treatments were considered only for the full-blown stages of illness (stage II and III). Stage subdivision criteria, according to Fontenelle and co-authors, were differentiated on the basis of illness course and pharmacological response. Stage II was divided into IIA (recurring trend) and IIB (persistent trend), while stage III was divided into IIIA (responsive to therapy) and IIIB (nonresponsive to therapy).
The model acknowledges that Y-BOCS is the most common assessment tool for OCD severity, and treatment choice is often based on Y-BOCS score thresholds.Reference Storch, De Nadai and Conceição Do Rosário 14 However, a univocal model considering all the clinically observable variables associated with OCD severity has not been defined yet. Storch and colleaguesReference Storch, De Nadai and Conceição Do Rosário 14 found a correlation between Y-BOCS scores and OCD severity, assessed through the Clinical Global Impressions-Severity scale (CGI). Particularly, Y-BOCS scores of 0 to 13 were correlated to “mild symptoms” (CGI-Severity = 0–2), scores between 14 and 25 to “moderate symptoms” (CGI-Severity = 3), scores between 26 and 34 with “moderate–severe symptoms” (CGI-Severity = 4) and scores between 35 and 40 with “severe symptoms” (CGI-Severity = 5–6). Mixed results were found for single items: time spent on obsessions/compulsions, interference, distress, resistance, and control were significantly related to global OCD severity, while symptoms resistance demonstrated a less robust correlation.Reference Storch, De Nadai and Conceição Do Rosário 14 Regarding clinical and sociodemographic variables, the results appeared to be less pronounced: neither age nor ethnicity was associated with Y-BOCS scores, but female patients showed more severe OC symptoms than males.Reference Storch, De Nadai and Conceição Do Rosário 14
Based on the above and with the intent to assess the potential clinical and therapeutic utility of a staging model in patients with OCD, defining potential predictors of improvement in recruited patients, the present study reports the preliminary results of its first application to an Italian sample of OCD patients attending two tertiary clinics.
Methods
In this prospective study, 60 OCD outpatients were recruited at the Psychiatry Unit 2 of ASST Fatebenefratelli-Sacco University Hospital of Milan and 10 OCD outpatients from Psychiatric service of “Circolo e Fondazione Macchi” Hospital of Varese from January 2018 to December 2019. All patients were diagnosed with OCD using the Structured Clinical Interview for DSM-5 (SCID-5).Reference First, Reed, Hyman and Saxena 16 All patients were receiving an appropriate pharmacological therapy for at least 1 month, chosen according to International treatment guidelines, given that the utility of psychopharmacological treatments for at least 12 weeks has been widely demonstrated in the OCD literature.Reference Hirschtritt, Bloch and Mathews 17 Exclusion criteria included: comorbidity with serious medical conditions, presence of an intellectual disability diagnosis, and comorbidity with other psychiatric disorders that may have caused OC symptoms as a secondary condition. The sample of patients who met the inclusion criteria was then clinically assessed. OCD severity was assessed using the Y-BOCS,Reference Koran, Hanna and Hollander 18 while the overall clinical status and the evolution of symptoms and general status were assessed through the CGI and the clinical interview.Reference Storch, Rasmussen and Price 19 Accurate epidemiological, physiological, and medical information were collected (see Table 1). Particular attention was paid to family history, history of pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections, other relevant medical conditions, history of substance use, age at onset and age at first psychiatric treatment, psychopharmacological treatments and psychotherapy, onset type (sudden or insidious), main phenotypes of obsessions/compulsions, and DUI. The latter was defined as the interval between symptoms onset and the administration of the first pharmacological treatment at standard dosage and for an adequate period of time. Patients’ sensitive data were collected anonymously, according to the Italian legislation (D.L. 196/2003, art. 110—July 24, 2008, art. 13) and in accordance with the ethical principles of the Declaration of Helsinki (with amendments) and Good Clinical Practice. All patients underwent a follow-up assessment between 12 and 24 months after the first visit and Y-BOCS and CGI scales were contextually administered.
Table 1. Sociodemographic Variables of the Study Sample at the End of Follow-Up observation.

Values for categorical and continuous variables are expressed in percentages and mean ± SD, respectively. Boldface indicates parameters with statistically significant differences between the two subgroups.
* P < .05.
** P < .01.
Staging groups
On the basis of their clinical features and Y-BOCS scores, patients were subdivided into the following staging groups: stage 0 for patients with Y-BOCS scores of 0 and positive family history for OCD; stage 1 for patients with Y-BOCS scores between 1 and 13; stage 2 included individuals with Y-BOCS scores between 14 and 34; patients with Y-BOCS scores higher than 35 were included on stage 3.
Patients were further subdivided after a 12 to 24 months period of follow-up according to Y-BOCS scores and clinical assessments: the first group included patients with unchanged stage between first and follow-up visit; the second group included patients with a stage improvement between first and follow-up visit, and the third group included patients with a worsened stage.
Statistical analysis
A descriptive statistical analysis of the main sociodemographic and clinical features of the sample was performed. Pearson Chi-squared test and one-way ANOVA analysis were used, respectively, for categorical and continuous variables. All analyses were performed using SPSS 24 for Windows software (Chicago, IL) and the level of statistical significance was set at 0.05.
Results
Sociodemographic and clinical variables of the sample are shown in Tables 1 and 2.
Table 2. Clinical Variables of Study Sample at the End of Follow-Up Observation.

Values for categorical and continuous variables are expressed in percentages and mean ± SD, respectively. Boldface indicates parameters with statistically significant differences between the two subgroups.
* P < .05.
** P < .01.
The whole sample was composed of 70 outpatients with a female rate of 44.3%. The mean age of the sample was 41.2 ± 13.4 years and the mean Y-BOCS score was 22.6 ± 8.5.
No significant sociodemographic differences were found between the two centers of Milan and Varese.
Considering the whole sample, at the first visit, 14.3% of patients belonged to stage 1, 74.3% belonged to stage 2, and 11.4% belonged to stage 3. During the follow-up assessment, 27.1% of patients belonged to stage 1, 67.1% of patients were assigned to stage 2, and 5.7% to stage 3.
On the basis of the comparison between Y-BOCS scores at the first and follow-up visits of each patient, the sample was divided into three groups: the first showed no stage changes and included 67.1% of patients; the second group included patients with an improved stage, accounting for 24.3% of the sample, while the third group included patients showing a worsened stage (8.6% of the whole sample). As regards the subgroup of patients with worsened stage, during the first visit a significant majority belonged to stage 1 (83.3%). In the improved stage group, during the first assessment, 70.6% of patients belonged to stage 2; and in patients with unchanged stage, 83% belonged to stage 2.
At the follow-up assessment, 83.3% of patients with stage worsening belonged to stage 2 while 16.7% belonged to stage 3. In the group with improved stage, 82.4% belonged to stage 1 and 17.6% to stage 2 (Table 2).
As concerns working status, patients belonging to the worsened stage showed higher rates of part-time employment and lower rates of full-time employment compared to patients with unchanged and improved stages (respectively 33.3% vs 2.1% vs 14.3%, P < .05; 0% vs 41% vs 42.9%, P < .05). No statistically significant differences were found in terms of gender distribution, mean age, psychopharmacological or psychotherapeutic treatments, suicidality, marital status, and education level within the three staging groups.
Patients with worsened stage compared to patients with unchanged stage and improved stage showed an earlier age at onset (25.3 ± 13.4 years vs 27.9 ± 10.5 years vs 27.9 ± 12.9 years), a longer DI (308.0 ± 120.2 months vs 239 ± 170.7 months vs 184.9 ± 151.2 months), and a longer DUI (141.0 ± 109.6 months vs 72.3 ± 99.5 and 68.6 ± 84.6 of unchanged stage and improved stage, respectively), although not reaching the statistical significance.
As regards psychiatric comorbidities, patients with worsened stage showed significantly higher rates of comorbid personality disorders with onset preceding OCD diagnosis, compared to patients with unchanged stage and improved stage (16.7% vs 0% vs 5.9%, respectively; P < .05). With respect to psychiatric comorbidities manifesting after OCD onset, all patients of the worsened stage group had comorbidities compared to patients with unchanged stage and improved stage (100.0% vs 61.7% vs 47%: P < .05%). In particular, the most significantly represented comorbidities of the worsened stage group compared to patients with unchanged and improved stages were bipolar disorder type 2 (BD II; 33.3%vs 2.1%vs 0%: P < .05), somatic symptoms and related disorders (SSD; 16.7% vs 0% vs 0%, P < .05), Eating Disorders (EBD; 16.7% vs 0% vs 5.9%: P < .05), and substance use disorders (33.3% vs 8.1% vs 12.5%, P < .05), alcohol use being the most represented (16.7% vs 2.7% vs 0%, P < .05) (Figure 1).

Figure 1. Significant psychiatric comorbidities after obsessive–compulsive disorder onset across stage groups. *P < .05.
Regarding obsessions phenotypes, in the worsened stage group, a significantly higher rate of patients showed somatic obsessions compared to patients with unchanged and improved stages (33.3% vs 29.8% vs 0%; P < .05), while the improved stage group showed significantly higher rates of magical thinking and violence/harm obsessions compared to unchanged and worsened stage groups (11.8% vs 0% vs 0%, P < .05; 23.5% vs 4.3% vs 16.7%, P < .05). No differences, in terms of compulsions phenotypes, emerged among the three subgroups (Figures 2).
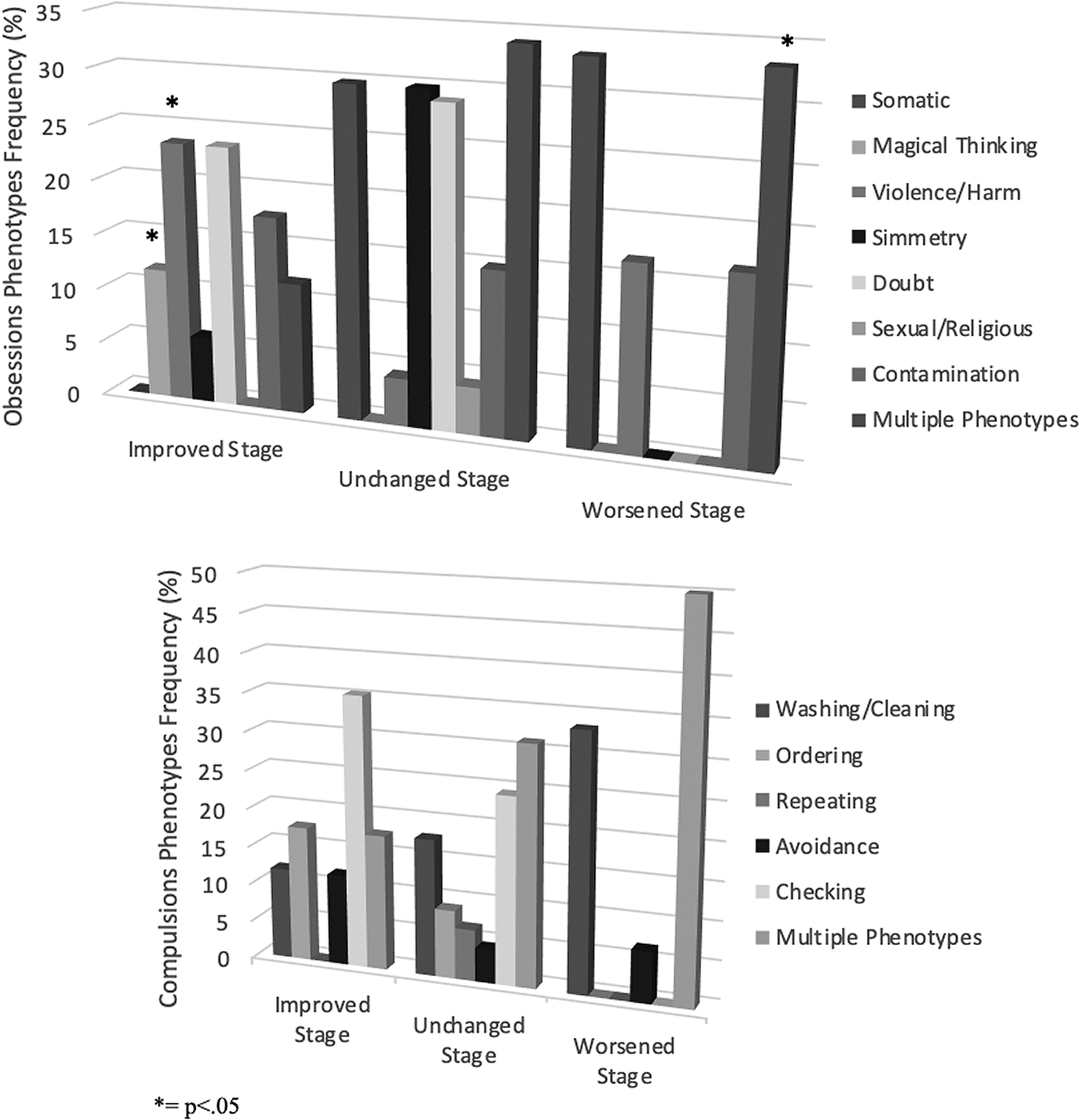
Figure 2. Main obsessions (a) and compulsions (b) Phenotypes across stage groups. *P < .05.
Discussion
Staging models proposed for psychiatric disorders are getting increasing interest in clinical practice.Reference Cosci and Fava 13 Such an approach may be applied to OCD as well, for the early identification of subclinical phases and early stages, in order to develop targeted therapeutic patterns consistent with a stepped-care approach.
To date, and to the authors’ knowledge, the present study was the first attempt to apply a staging model in a clinical sample of OCD patients. The aim of the present study was to define potential features of clinical improvement through a new staging model for OCD patients.
From a first epidemiologic point of view, stage 2 included the largest number of patients at the time of the first assessment, being, among the four stages, the group comprising the widest values of Y-BOCS scores, as previously described.Reference Fontenelle and Yücel 15 At the follow-up visit, the majority of patients was still in stage 2, but the rates of the different stages changed as follows: patients belonging to stage 2 and stage 3 decreased, in favor of patients belonging to stage 1, that had doubled, suggesting a global improvement of the sample, probably due to an efficacious response to prescribed psychopharmacological treatment. Patients presenting a clinical worsening mainly belonged to stage 1—that is, first visit Y-BOCS scores ranging from 1 to 13—showing that a previous mild symptomatology was not necessarily predictive of a better outcome. Moreover, unchanged patients were mostly represented in stage 2, highlighting, in the present sample, a greater clinical stability—or chronic symptomatology—associated to moderate symptomatic features in OCD patients. Taken as a whole, these results underlined how targeted treatment may improve the clinical picture, being OCD a disease with a mainly chronic course, but positively influenced by pharmacological treatment. Other authors showed that even more serious stages may be considered as expressions of temporary exacerbations of the disorder and not as a stable condition.Reference Sharma and Math 10 Ultimately, a notable consideration is that the application of a staging model to OCD patients reveals that patients can indeed move bidirectionally through different stages during a follow-up observation period.
Present data showed many associations of clinical and phenotypic features with staging progressions. Among the most important, the age at onset seemed inversely related to staging negative progression, while DI and DUI would be directly related. Despite not reaching the statistical significance in our sample, observed findings are consistent with the available literature.Reference Vigne, Fortes and Dias 2 In addition, other sociodemographic variables might be worthy of consideration for a staging model. Our sample showed that patients with a full-time job more frequently belonged to a milder severity stage, while patients with a part-time job were mostly represented in the worsened stage. This difference could be explained by the greater disability associated with more severe stages: OCD severity and social/financial difficulties, in fact, have already been positively correlated in previous reports.Reference Busner and Targum 20
Another variable potentially involved in stage worsening was represented by the pre- and post-OCD onset comorbidity. Of note, in the worsened stage group, all patients had at least one comorbid condition after the OCD onset. This is consistent with published investigation identifying the presence of comorbidities as a negative prognostic factor.Reference Hollander, Doernberg and Shavitt 21 In particular, psychiatric comorbidities could represent, on one hand, an obstacle for the overall management (i.e., for diagnosis and treatment) of patients and, on the other hand, a longitudinal characteristic of worse progression and poor outcome in OCD. In the present sample, a significantly higher prevalence of BD II, EBD, SSD, substance use disorders, and personality disorders was found in the worsened stage group.
The association between bipolar disorder and OCD was recently analyzed—in a previous study from our group assessing a large international OCD sample. Results showed that 6.2% of OCD patients had a comorbid bipolar disorder, which is significantly associated with greater severity of OC symptoms, poly-pharmacotherapy, and previous hospitalizations.Reference Van Oudheusden, Eikelenboom and van Megen 22 In this study, the diagnosis of BD II was, in most cases, chronologically subsequent to that of OCD, and this might be partly explained by the use of SSRIs/SNRIs for the treatment of OCD (at high dosages),Reference Dell’Osso, Vismara and Benatti 23 with the consequent development of hypomanic symptoms in predisposed patients. As a consequence, the presence of hypomanic symptoms/episodes in these patients could limit the pharmacological options for the treatment of OCD, resulting in a worse clinical outcome.Reference Dell’Osso, Mundo and Marazziti 24
The association between OCD and EBD has been previously highlighted in the literature, but the etiopathogenesis has not been elucidated yet.Reference Perugi, Toni and Frare 25 The pre-onset presence of an EBD in our sample was found to be significantly more prevalent in the OCD group with worsened stage. This could be explained with the tendency of these particular patients to refuse drugs that could cause weight gain, such as antidepressants and antipsychotics, with a consequent OCD symptom worsening. The presence of SSD has already been associated with scarce insight and psychiatric comorbidities,Reference Cederlöf Poyraz, Turan and Sağlam 26 supporting our findings and encouraging future investigation in the field.
The consumption of abuse substances after OCD onset appeared significantly related to stage worsening. The comorbidity between OCD and substance abuse has been, to date, poorly investigated, although some studies have shown higher prevalence of substance consumption in OCD patients, compared to the general population as well as a higher prevalence of OCD in patients with a primary diagnosis of substance use disorder.Reference Jakubovski, Diniz and Valerio 27 , Reference Blom, Koeter and van den Brink 28 There is evidence showing that comorbidity with substance abuse was related to more severe clinical features, greater social impairment, and a higher number of suicidal attempts.Reference Blom, Koeter and van den Brink 28 The significantly higher prevalence of substance abuse occurring after OCD onset could be interpreted in light of a common biological basis of compulsive and impulsive behaviors leading, over time, to an overlap of compulsions with more impulsive behaviors, while addiction behaviors would convert in mechanisms of habit and, therefore, compulsivity.Reference Fontenelle and Yücel 15 , Reference Mancebo, Grant and Pinto 29 Another possible explanation would be that the presence of substance and alcohol abuse could reduce control over obsessions and compulsions, thus determining a worse clinical picture.Reference Fontenelle and Yücel 15
Lastly, the psychiatric comorbidities with personality disorders were more frequently associated to the worsened stage. Comorbid personality disorders have been consistently associated with a poor illness outcome and scarce treatment response.Reference Thamby and Khanna 30 In particular, borderline personality disorder has been previously proposed as part of a wider obsessive–compulsive spectrum of disorders. Within the obsessive–compulsive spectrum of disorders, each disorder may be located on a continuum of different conditions on the basis of specific symptom dimensions. For example, on the harm avoidance/risk-seeking dimension, obsessive–compulsive disorder would represent the condition that overestimates potential harm on one end of the spectrum, while borderline personality disorder would fit in on the opposite end, as patients with this disorder appear to underestimate potential harm and act impulsively, taking unnecessary risks.Reference Dell’Osso, Berlin and Serati 31
Finally, the obsessive phenotype seems to represent another important variable for staging progression, as some specific phenotypes in our sample showed a stronger correlation with the OCD severity trend. In particular, in the group with improved stage, obsessions with violent/aggressive content and magical thinking significantly prevailed. A possible explanation is that, being in obsessions is a highly disturbing and egodystonic experiences, even a minimal reduction of them could be perceived at a subjective level with considerable relief, therefore justifying a stage improvement. Conversely, somatic obsessions seem to correlate with a worse prognosis. A possible hypothesis in this respect could be that these specific patients may show a lower insight and, therefore, a minor adherence to prescribed treatments.Reference Marazziti and Dell’Osso 32
The present study being the first report for applying a staging approach to OCD patients, the following methodological limitations should be kept into consideration. One of the limitations is the relatively small sample size of enrolled patients. A further analysis with a larger sample is warranted. In addition, the staging interval should include a longer period of observation, with repeated assessments; a specific focus on the follow-up of patients from the time of their psychopharmacological treatment initiation for a more accurate prognostic definition should be considered. Moreover, it is relevant to underline that anamnestic analysis, although precise, could not be completely free from recall bias. In addition, given the prescription, for each patient, of a psychopharmacological treatment, we cannot derive any data concerning the naturalistic course of OCD for those patients. Lastly, staging models could be revised in terms of more stringent defining features for each stage. However, the briefness and clarity of the tools used in the present study, such as the Y-BOCS, resulted in a good adherence and compliance to the follow-up plan.
Acknowledgements
None.
Funding
None to declare.
Conflict of Interests
Beatrice Benatti, Giulia Lucca, Riccardo Zanello, Fabio Fesce, Alberto Priori, Nicola Poloni, Camilla Callegari, Leonardo F. Fontenelle, and Bernardo Dell’Osso declare no competing conflict of interests.