Introduction
In the past years a growing body of evidence suggested that obsessive-compulsive disorder (OCD) patients display increased impulsivity, impaired decision-making, and reward system dysfunction.Reference Prochazkova, Parkes and Dawson1–Reference Chamberlain, Fineberg and Menzies7 In a Research Domain Criteria (RDoC) (www.nimh.nih.gov) perspective, these findings are prototypical for addiction and recently have led some authors in the past years to view OCD as a behavioral addiction. In this perspective, comparable to addiction, OCD is perceived as process, in which patients with OCD develop over time a dependency upon their compulsive behaviors because of the rewarding effect when performed perfectly or when compulsions reduce obsession-induced anxiety or distress.Reference Denys8 Indeed, a recent study showed that compulsive behaviors in OCD are reward-driven, as is the case for addictive behaviors.Reference Ferreira, Yücel and Dawson9
Recently, we investigated the behavioral addiction model of OCD, by assessing two core dimensions of addiction, namely, impulsivity and decision-making, in OCD patients and healthy participants. Similar to common findings in addiction, OCD patients demonstrated increased cognitive impulsivity and impaired decision-making compared to HCs.Reference Grassi, Figee and Ooms2
Gambling disorder (GD), which is included in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5, American Psychological Association, 2013) in the substance-related and addictive disorders chapter, represents the prototype of a behavioral addiction. In an RDoC perspective, increased impulsivity, risky decision-making, and reward system dysfunction represent three core dimensions of GD.Reference Grant, Odlaug and Chamberlain10 However, no studies directly compared OCD and GD patients on these three core features of both disorders to date.
Investigating these RDoC networks across OCD and GD could be relevant in moving forward the current OCD models, mainly focused on anxiety and compulsivity, highlighting the relevance on other RDoC dimensions such as inhibitory control networks (impulsivity), decision-making processes, and reward system dysfunctions, as putative treatment targets for OCD.
The goal of the present study was to investigate similarities and differences on impulsivity, decision-making, and reward system, as core dimensions of addiction, across OCD patients and GD patients. Based on published reportsReference Figee, Vink and de Geus5, Reference Denys8 and our previous observations,Reference Grassi, Pallanti and Righi3 we hypothesized that OCD patients, similar to GD patients, show increased impulsivity, impaired decision-making, and reward system dysfunction as compared to healthy controls (HCs).
Methods
Participants
Forty-four OCD patients, 26 GD patients, and 40 HCs were included in the study. Patients were recruited from the Impulsive-Compulsive Disorders Unit of the University of Florence, between 2014 and 2015. HCs were recruited by advertisements and word of mouth. All groups were matched for sex and age. Both the OCD group and the GD group had a primary diagnosis of OCD and GD, respectively.
Inclusion criteria for both patient groups were: (1) presence of DSM-IV criteria for OCD or GD, established by a psychiatrist and confirmed by the Structured Clinical Interview for DSM-IV Axis-I Disorders/Patient Edition (SCID-I/P)Reference First, Spitzer, Gibbon and Williams11 and (2) age between 18 and 65 years.
We excluded potential patients with any of the following conditions: (1) current DSM-IV Axis I diagnosis of a mood episode or current substance-related disorders (except for nicotine addiction), schizophrenia or other psychotic disorders, Tourette’s disorder; (2) any primary Axis II clinical diagnosis (established by a clinical interview conducted in accordance with the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) flow-chart)Reference First, Gibbon and Spitzer12; (3) episodic OCD (this criterion was selected in order to avoid misdiagnosed bipolar spectrum disorder patients); (4) illness duration less than 2 years; (5) hospitalization in the past 6 months; (6) pharmacological treatment changes in the past 4 weeks; (7) mental disorder due to a general medical condition or history of mental retardation.
HCs did not have any history of psychiatric disorders or a family history of OCD or GD, as confirmed by the SCID-I/NP (Non-patient Edition).Reference First, Spitzer and Gibbon13 Demographic and clinical variables of all subjects are displayed in Table 1.
TABLE 1. Clinical and demographic variables

Note: Data are expressed as percentage for categorical variables or median (interquartile range) for continuous variables.
Values in bold are the statistical significant p values.
// refers to the fact that there is no information about this variable for the control group.
OCD and GD patients with lifetime comorbid psychiatric disorders were not excluded from the study since OCD and GD was, respectively, the dominant pathology and the reason for seeking treatment. In the OCD group 12 out of 44 patients (27.3%) had a history of lifetime comorbid psychiatric disorders: major depressive disorder (6 patients), anxiety disorders (2 patients, panic disorder; 2 patients, social anxiety disorder), OCD spectrum disorders (1 patient, body dysmorphic disorder; 1 patient, hoarding disorder), chronic tic disorders (4 patients). In the GD group 15 out of 26 patients (57.7%) had a history of lifetime comorbid psychiatric disorders: mood disorders (5 patients, bipolar spectrum disorders; 4 patients, major depressive disorder), substance use disorders (2 patients, alcohol use disorder; 1 patient, cocaine use disorder), anxiety disorders (2 patients, panic disorder; 1 patient, social anxiety disorder).
In the OCD group 41 out of 44 patients (93.2% of the total sample) were under ongoing medications. Thirty-one patients were taking serotonin-reuptake inhibitors (SRIs) medications only (citalopram, escitalopram, fluvoxamine, fluoxetine, paroxetine, sertraline, or clomipramine), and 10 patients were taking SRIs plus antidopaminergic medications (risperidone or aripiprazole). Twenty patients out of the whole OCD sample were undergoing a cognitive-behavioral therapy. In the GD group 16 out of 26 patients (61.5% of the total sample) were under ongoing medications. Six patients were taking SSRIs medications (paroxetine, sertraline, and citalopram), while 10 patients were taking mood stabilizers (valproate, lithium, topiramate).
Potential subjects in both groups with conditions that potentially could affect the nasal epithelium functions and therefore odor detection abilities were excluded. Thus, we excluded subjects suffering from any significant olfactory symptoms, such as those associated with the common cold, influenza, nasal allergies, or any organic conditions such as upper respiratory tract infection (rhinosinusitis, polyposis, allergic rhinitis) or patients who had undergone surgery on the nasal septum, turbinates, or paranasal sinuses. Also, we excluded patients with a history of any systemic condition that could affect olfaction abilities such as chronic obstructive pulmonary disease, asthma, active hepatitis, cirrhosis, chronic renal failure, vitamin B12 deficiency, cerebral vascular accidents, insulin-dependent diabetes mellitus, hypothyroidism, and Cushing syndrome.
Smokers were included in the study, although none of the subjects was permitted to smoke in the hour immediately preceding the olfactory examination.
The study procedures were carried out in accordance with the Declaration of Helsinki. The study was approved by the institutional review board of the University of Florence, and all participants had to sign the informed consent to be included in the study. All procedures were done in one day.
Procedures and assessments
Clinical assessments
OCD and GD symptoms’ severity was assessed by independent evaluators using the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS)Reference Goodman, Price and Rasmussen14, Reference Goodman, Price and Rasmussen15 and the Yale-Brown Obsessive-Compulsive Scale adapted for Pathological Gambling (PG-YBOCS),Reference Pallanti, DeCaria and Grant16 respectively. Both scales have a score range of 0–40, with higher scores representing greater severity. To assess OCD symptoms subtype we used the Y-BOCS symptoms checklist (Y-BOCS-SC). On the basis of the Y-BOCS-SC, patients’ primary symptoms were classified as one of five a priori dimensions based on factor analysis performed on previous studiesReference Brakoulias, Starcevic and Berle17: (1) doubt/checking, (2) contamination/cleaning, (3) symmetry/ordering, (4) unacceptable/taboo thoughts, and (5) hoarding. GD patients’ primary symptoms were classified according to gambling type as one of the following five dimensions: (1) slot machines, (2) lottery, (3) bets, (4) card games (including online games), and (5) casino.
We also performed a clinical interview in order to assess social and demographic variables, duration of illness, current pharmacological or CBT treatments. Clinical variables of OCD and GD subjects are displayed in Table 1.
The presence of anxiety and depression symptoms was assessed through the Hamilton Anxiety Rating Scale (HAM-A)Reference Hamilton18 and the Hamilton Depression Rating Scale (HAM-D-17 items),Reference Hamilton19 respectively.
Patients’ and controls’ intelligence was assessed through the Italian version of the National Adult Reading Test (Test di Intelligenza Breve, TIB).Reference Sartori, Colombo and Vallar20 The TIB consists of 54 words (34 effective test-words with irregular accent and 20 control-words with high frequency of use) that subjects have to read and pronounce. The total number of mistakes of reading defines the TIB error score. The estimated IQ scores (i.e., performance, verbal, and total) are calculated through the regression of equations taking into account sex, age, and educational level. The variables we used in the statistical analysis were estimated total IQ, estimated performance IQ, and estimated verbal IQ.
In order to control olfaction assessment for smoking status we assessed nicotine dependence through the Fagerstrom Test for Nicotine Dependence (FTND), a widely used test to assess several different nicotine addiction dimensions including the number of smoked cigarettes per day.Reference Heatherton, Kozlowski and Frecker21
Impulsivity assessment
Impulsivity traits were assessed using the Barratt Impulsiveness Scale, version 11 (BIS-11). This scale consists of 30 self-descriptive items, with responses in a four-point Likert-type scale ranging from “Rarely/Never” to “Almost Always/Always.”Reference Patton, Stanford and Barratt22 It measures the total score (range: 30–120) of impulsivity and three factors: Attentional Impulsiveness (AI), Motor Impulsiveness (MI), and Non-planning Impulsiveness (NPI) with higher scores indicating higher impulsivity. BIS-11 was used in its Italian translation.Reference Fossati, Di Ceglie and Acquarini23
Decision-making assessment
To assess decision-making, we used the Iowa Gambling Task (IGT), a card game that is widely used to study decision-making under ambiguity conditions (the probability of different outcomes is unknown).Reference Brand, Labudda and Markowitsch24, Reference Brand, Recknor and Grabenhorst25 Decision-making behaviors on the IGT can separate “risky-players” that prefer immediate reward despite negative future consequences, from “risky-avoidant” players that prefer small but long-term rewarding choices.Reference Cavedini, Zorzi and Baraldi26 In the IGT the subject must make 100 card selections from four decks (A, B, C, and D), and the objective is the maximum profit. At the beginning of the test the subjects receive a loan of play-money. After turning over each card, subjects are either given money or asked to pay a penalty according to a programmed schedule of reward and punishment. Gains and losses are different for each deck. Decks A and B (disadvantageous decks) are high paying but disadvantageous in the long run, because the penalties are even higher. Decks C and D (advantageous decks), on the other hand, are low paying but advantageous because the penalties are lower, resulting in an overall gain in the long run. In this study, we used a computerized version of the original IGT.Reference Bechara, Damasio and Damasio27–Reference Tomassini, Struglia and Spaziani29 The performance was measured using the netscore, defined by choices from advantageous (C and D) minus disadvantageous (A and B) decks, with higher scores indicating a risk-avoidant pattern of decision making. The netscore for each block of 20 cards was also considered in order to evaluate the choice behavior during the task. We considered the first and second blocks as decisions under ambiguity (the probability of outcome is unknown during these blocks of choices) while we considered the third, fourth, and fifth blocks as decisions under risk (subjects learn how the decks work during the first and second block, and thus the probability of outcome is known during these blocks of choices).
Reward system assessment
In order to investigate reward system functioning we assessed hedonic tone through a self-report clinical instrument and through an olfactory test assessing hedonic appraisal to odors. Indeed, several studies suggested that exposure to pleasant and/or aversive odors activates key structures of the human reward system, and abnormalities of human reward system functioning may be probed by olfactory stimuli.Reference Anderson, Christoff and Stappen30, Reference Fagundo, Jiménez-Murcia and Giner-Bartolomé31 Thus, abnormal hedonic appraisal to odors has been showed in psychiatric disorder characterized by reward system dysfunctions, such as schizophrenia.Reference Mesholam-Gately, Gibson and Seidman32
Anhedonia assessment
To assess hedonic tone, we used the Snaith–Hamilton Pleasure Scale (SHAPS).Reference Snaith, Hamilton and Morley33 The SHAPS is a 14-item self-report instrument designed to assess hedonic tone. Participants are presented with 14 statements of enjoyable activities (e.g., “I would be able to enjoy my favorite meal,” “I would enjoy a warm bath or a refreshing shower.”) and must choose one of four optional responses: Definitely Agree, Agree, Disagree, and Strongly Disagree. Each of the Agree responses receives a score of 0, and each of the Disagree responses receives a score of 1. The SHAPS total score ranges from 0 to 14 with higher scores reflecting greater anhedonia severity. According to criteria established by Snaith and colleagues, a cutoff score of more than two negative responses determines the presence of clinically significant anhedonia. In the present study, we used the Italian validated version of the SHAPS.Reference Santangelo, Morgante and Savica34
Odor hedonic task
Patients were presented with three odor sticks from the 12 sticks of the Burghart’s Sniffin’ Sticks Screening Test.Reference Steinbach, Hummel and Böhner35 The three sticks represented a “pleasant,” a “neutral,” and an “unpleasant” odor, respectively. Based on the data of a previous investigation on 10 male and 10 female healthy volunteers aged 18–65 years, the rose odor stick, the leather odor stick, and the fish odor stick were used as the pleasant, neutral, and unpleasant odors, respectively. The pleasant odor was always presented first in order to avoid possible carryover effects of the more enduring unpleasant stimulus. Then, they were presented with the neutral odor, followed by the unpleasant odor. Participants were exposed to each odorant for 30 s with 1 min in-between each of the odors. Participants rated the intensity and hedonic valence of each odor by pointing to a specific value on a visual analog scale. The range of the valence scale was from −7 (extremely unpleasant) to +7 (extremely pleasant).
In order to avoid potential confounding effects on pleasantness and unpleasantness patients’ ratings, olfactory identification abilities were assessed using the Burghart’s Sniffin’ Sticks Screening Test.Reference Steinbach, Hummel and Böhner35 The test employs 12 odorant pens and requires the subject to choose among four written alternatives for each odorant. Reachable scores are 0–12 (higher scores indicate a better ability of odor identification). The order of olfactory testing was the same for all participants. For odor presentation, the cap was removed for 3 s, and the pen’s tip was placed 2 cm in front of the nostrils. The inter-stimulus interval was at least 20 s to prevent olfactory desensitization. Olfactory tests were administered birhinally in a quiet, well-ventilated room to avoid any background smell interfering with the test odors.
Statistical analyses
Normality of all variables was evaluated using the Shapiro–Wilk test. Non-normally distributed variables were sex, age, years of education, estimated total IQ, performance IQ, verbal IQ, illness duration, BIS attentional and motor subscale, BIS total score, odor identification score, pleasurable, neutral, and aversive odor scorings, IGT netscore 1,2,3,4, and 5, FTND score, HAM-D, HAM-A, PG-YBOCS, and Y-BOCS. The only normally distributed variables were the BIS Non-planning subscale and the IGT total netscore. Since most of examined variables were not normally distributed, non-parametric tests were used. Primary outcomes were impulsivity score (measured by the BIS-11), decision-making performance (measured by the IGT), and hedonic tone measure (measured by the SHAPS and odor hedonic task). Kruskal–Wallis rank sum test was used to compare continuous or interval variables between the three groups, while chi-square test was used for categorical variables. Bonferroni adjustment was used for all post-hoc analyses. Spearman’s rank correlation test (in order to correlate continuous and dichotomous variables) was used to evaluate the interaction of demographic and clinical variables (age, sex, educational attainment, IQ scores, nicotine dependence, gambling type or OC symptoms subtype, illness duration, history of tics, and presence of comorbidity and/or medications) and primary outcome measure (impulsivity, decision-making, and hedonic tone measures). Level of significance was set at p = 0.05. All analyses were carried out using the Statistical Package for the Social Sciences v25 (SPSS).
Results
Demographic and clinical characteristics
There were no significant differences between the three groups with regard to sex and age (see Table 1). The three groups differed on years of education (χ2(2) = 14.364, p = 0.001). Post-hoc test revealed that GD patients had a lower educational attainment (median 12.5) than OCD patients (median 13, p = 0.004) and HCs (median 13, p = 0.001) while no significant differences were found between OCD patients and HCs (see Table 1). However, the three groups did not differ on total IQ measures (p = 0.085) and performance IQ (p = 0.474), and they only differed on verbal IQ (χ2(2) = 9.903), p = 0.007) (GD patients showed significantly lower scores (median 103.66) than OCD patients (median 108.65, p = 0.034) and HCs (median 109.59, p = 0.007), while no differences were observed between OCD patients and HCs). The three groups differed on Fagerstrom test scores (χ2(2) = 11.954, p = 0.003), and GD patients (median 2.5) showed significant higher scores than OCD patients (median 0, p = 0.003) and HCs (median 0, p = 0.013), while OCD patients and HCs did not show significant differences (see Table 1).
The three groups differed on odor identification abilities (χ2(2) = 20.564, p < 0.001). Both OCD (median 10.5) and GD (median 10) showed significantly lower scores than HCs (median 11) (p = 0.019 for OCD vs HCs and p < 0.001 for GD vs HCs), while OCD and GD did not differ (p = 0.096).
As expected the three groups differed on anxiety (χ2(2) = 39.638, p < 0.001) and depressive symptoms (χ2(2) = 42.031, p < 0.001) (see Table 1). GD and OCD patients showed higher scores on both HAM-D and HAM-A scales when compared to HCs (p < 0.001 for both tests), but no statistically significant difference was found between them. Also, we found a significant difference between the three groups on obsessive-compulsive symptoms assessed with the Y-BOCS and gambling symptoms assessed with the PG-YBOCS (χ2(2)=89.675, p < 0.001 and χ2(2)=86.479, p < 0.001 respectively). As expected, GD patients showed significantly higher PG-YBOCS scores than the other groups (p < 0.001), while OCD and HCs did not show differences and OCD patients showed higher Y-BOCS score than the other groups (p < 0.001), while GD and HCs did not differ.
OCD and GD patients did not differ on illness duration (χ2(2)=2.969, p = 0.085), while they differed on comorbidity rates (χ2(2)=6.383, p = 0.012) and proportion of medicated patients (χ2(2)=10.821, p = 0.001) (see Table 1).
Impulsivity measure results
The three groups significantly differed on BIS-11 total score and all the BIS-11 subscales (χ2(2)=23.007, p < 0.001 for BIS-11 total score, χ2(2)=28.049, p < 0.001 for BIS-11 Attentional subscale, χ2(2)=11.487, p = 0.003 for BIS-11 motor subscale and χ2(2)=9.989, p = 0.007 for BIS-11 Non-planning subscale) (see Table 2). Post-hoc test revealed that both OCD (median 67, p < 0.001) and GD (median 68, p < 0.001) patients scored significantly higher than HCs (median 58) on BIS-11 total score, while no statistically significant differences were found between OCD and GD patients. Concerning BIS-11 subscales, post-hoc test showed that both OCD and GD patients showed significant higher scores on BIS-11 attentional subscale (median 19, p < 0.001 for OCD and 13 for GD, p = 0.006) than HCs (median 13), but no differences were found between OCD and GD groups (p = 0.4). On the other hand, GD patients showed significantly higher scores on BIS-11 motor subscale (median 22.5) than HCs (median 19, p = 0.002), while no differences were observed between GD and OCD (median 21, p = 0.122) and OCD and HCs (p = 0.335). Also, GD patients showed significantly higher scores on BIS-11 non-planning subscale (median 31.5) than HCs (median 25, p = 0.007), while no differences were observed between GD and OCD (median 27, p = 0.761) and OCD and HCs (p = 0.085).
TABLE 2. Impulsivity, decision-making, and reward measures across OCD, GD, and HCs

Note: Data are expressed as percentage or median (interquartile range) for all variables.
Decision-making performance results
The three groups showed a significant difference on IGT total Net score (χ2(2) = 24.877, p < 0.001). Post-hoc test revealed that IGT total Net score was statistically significantly lower in OCD (median 9, p < 0.001) and GD patients (median 3, p < 0.001) compared to HCs (median 22) (see Table 2), while there was no statistically significant difference between OCD and GD groups. Regarding the five IGT blocks series the three groups did not show significant differences on block 1 and 2 (putatively representing decision-making performance under ambiguous conditions), while they differed on blocks 3, 4, and 5 (putatively representing decision-making performance under risky conditions) (see Table 2). On block 3, 4, and 5 both OCD (median 0, p = 0.013, 2, median 2, p = 0.008 and median 0, p < 0.001, respectively) and GD patients (median 0, p = 0.013, median 2, p = 0.006 and median 2, p = 0.014, respectively) showed significantly lower netscores than HCs (median 4, 6, and 7 respectively) (see Table 2). However, OCD and GD patients did not differ on blocks 3 (p = 0.401), 4 (p = 1.000), and 5 (p = 0.241) (see Table 2).
Reward system results
The three groups significantly differed on SHAPS scores (χ2(2) = 31.876, p < 0.001). Post-hoc test revealed that both OCD (median 1.25, p < 0.001) and GD (median 3, p < 0.001) patients showed higher anhedonia scores than HCs (median 0), while no significant differences emerged between OCD and GD patients (p = 0.333). Percentage of presence of significant anhedonia (SHAPS score higher than 2) was 53.8% for GD (14 out of 26 patients), 40.9% for OCD (18 out of 44 patients), and 0% for HCs (0 out of 40 subjects).
Depressive, anxiety, and OC or GD symptoms scores did not correlate with SHAPS scores for GD patients, while moderate positive correlations were found between depressive, anxiety, OC symptoms, and SHAPS scores for OCD patients (for HAM-D rs = 0.358, p = 0.017; for HAM-A rs = 0.384, p = 0.010; for Y-BOCS rs = 0.389, p = 0.049).
Concerning subjects’ response to pleasant, neutral, and unpleasant odors, the three groups significantly differed on pleasant odor ratings (χ2(2) = 11.856, p = 0.003), while they did not differ on both neutral (χ2(2) = 5.573, p = 0.062) and unpleasant (χ2(2) = 3.036, p = 0.219) odors ratings. Post-hoc test showed that GD patients showed significantly lower ratings (median 3, p = 0.002) for the pleasant odor than HCs (median 5), while no difference were observed between OCD (median 4, p = 0.110) and HCs and OCD and GD patients (p = 0.327). Both odor identification abilities and smoking status/nicotine dependence did not correlate with odor pleasantness rating for OCD, GD, and HC groups.
Correlation analyses
When we looked at correlation between clinical demographic and clinical characteristics and primary outcome measures, we found several correlations. GD and OCD patients differed on comorbidity rates and medicated patient’s rates. However, the presence of comorbidity did not correlate with any primary outcome measure for both OCD and GD patients, and the presence of ongoing medications only correlated with unpleasant odor rating but patients did not differ from controls on this measure. The most clinically relevant correlations observed in the patients’ groups were as follows: in the OCD group, for impulsivity measures, BIS-11 total score positively correlated with HAM-D scores (rs = 0.350, p = 0.020), HAM-A scores (rs = 0.319, p = 0.035), and SHAPS score (rs = 0.402, p = 0.007), while in the GD group, BIS-11 total score positively correlated with PG-YBOCS score (rs = 0.453, p = 0.020). Depression, anxiety, and OC symptoms positively correlated with SHAPS score in the OCD group (for HAM-D rs = 0.358, p = 0.017; for HAM-A rs = 0.384, p = 0.010; for Y-BOCS rs = 0.389, p = 0.049), while this was not the case in the GD group.
Although antidopaminergic medications could affect reward and decision-making networks, when we compared OCD patients treated with antidopaminergic agents (10 patients) and OCD patients treated with SRIs and/or CBT only we did not find any difference on primary outcome measures.
Discussion
The main finding of this study is that OCD patients display several similarities and some differences with GD patients on impulsivity, decision-making, and reward functioning, the three core dimensions of substance and behavioral addictions, when compared to HCs. Specifically, both OCD and GD patients showed increased impulsivity when compared to HCs, but for OCD patients this difference was driven by increased cognitive impulsivity, while for GD patients it was driven by both cognitive and motor impulsivity. Furthermore, both OCD and GD patients showed impaired decision-making performances when compared to HCs. Finally, GD patients showed increased anhedonia and blunted hedonic response to pleasant odors unrelated to gambling or depression/anxiety symptoms, while OCD patients showed only increased anhedonia levels related to OC and depression/anxiety symptoms. To the best of our knowledge, this is the first study investigating impulsivity, decision-making, and reward system across OCD and GD patients.
Our impulsivity results are in line with previous literature showing that OCD patients display higher cognitive impulsivity than HCs on the BIS-11 scale,Reference Grassi, Figee and Ooms2, Reference Benatti, Dell’Osso and Arici4, Reference Ettelt, Ruhrmann and Barnow36 and with previous studies showing both cognitive and motor impulsivity as core features of GD patients.Reference Chowdhury, Livesey and Blaszczynski37 Indeed, both OCD and GD patients showed increased impulsivity than HCs but differently driven by cognitive and both cognitive and motor impulsivity, respectively. Of note, some studies assessing motor impulsivity in OCD patients through a behavioral task (stop signal task) showed increased motor impulsivity than to HCs.Reference Chamberlain, Fineberg and Menzies7 Therefore, it could be hypothesized that the BIS-11 scale is not sensitive or specific enough to capture motor impulsivity features in OCD patients. Thus, further studies comparing OCD and GD patients on motor impulsivity through behavioral tasks are needed in order to elucidate similarities and differences between OCD and GD on motor impulsivity.
Decision-making results in our study are largely in line with previous literature showing impaired performances on the IGT when compared to HCs for both OCD and GD patients.Reference Grassi, Figee and Ooms2, Reference Grassi, Pallanti and Righi3, Reference Cavedini, Zorzi and Piccini6, Reference Cavedini, Zorzi and Baraldi26, Reference Kovács, Richman and Janka38 In our sample both OCD and GD patients showed impaired decision-making performances than HCs and specifically they performed worse than controls on the last three blocks of cards, putatively assessing decision-making under risky conditions. However, it is still debated if the IGT is really able to distinguish decision-making under ambiguity and under risk, and therefore it is mainly considered a decision-making task under ambiguous conditions. Moreover, previous studies on OCD patients comparing decision-making performances under ambiguity and under risk with different tasks did not find impaired performances under risky conditions.Reference Zhang, Dong and Ji39
Finally, results from reward system assessment (self-report of anhedonia symptoms and odor hedonic task) showed that both GD and OCD patients showed the presence of a reward dysfunction. However, this reward dysfunction seems to be differently mediated in GD and OCD patients. Indeed, both OCD and GD patients display higher anhedonia symptoms scores than HCs. However, while GD patients’ anhedonia symptoms were independent by gambling symptoms, depression, and anxiety symptoms, OCD patients’ anhedonia symptoms were correlated to OC symptoms, depression, and anxiety symptoms. These results on OCD patients are in line with a previous study showing high anhedonia ratings in OCD positively correlated with severity of OC symptoms. However, contrary to our results, in this previous study the anhedonia scores of OCD patients were not correlated to depressive symptoms.Reference Abramovitch, Pizzagalli and Reuman40 In that study, the authors used our same instruments (the HAM-D and the SHAPS) to assess anhedonia and depressive symptoms; however, the sample was larger than our sample (more than hundred patients). Thus, we cannot rule out the hypothesis that our results differed from those of that study because we were underpowered on that outcome.
Also, in the odor hedonic task, GD patients showed significantly lower hedonic ratings to the pleasant odor when compared to both OCD and HCs, while OCD patients did not differ from HCs. These results seem to be in line with neuroimaging studies investigating reward system in OCD and GD patients. In fact, while imaging study consistently showed both anticipatory and consummatory reward dysfunction in GD,Reference Luijten, Schellekens and Kühn41 imaging studies on OCD showed mainly a reward anticipation dysfunction.Reference Figee, Vink and de Geus5 Thus, since our instruments assessed mainly consummatory reward (hedonic tone and hedonic response to pleasant odors), further investigations of both anticipatory and consummatory reward functioning in GD and OC are needed in order to elucidate commonalities and differences.
Several limitations are worth of mentioning. First, we investigated reward system by two instruments (a self-report anhedonia symptoms scale and the odor hedonic task) that putatively assess only consummatory reward, instead of both reward anticipation and reward consumption. Thus, we were not able to further investigate putative similarities and differences between different reward circuitries across these two disorders. Also, we did not use any behavioral measure of impulsivity, and therefore we could not exclude the presence of some commonalities on behavioral inhibition that the BIS-11 did not capture between OCD and GD patients. Finally, we did not assess patients’ functioning and disability, and thus we could not speculate on how differently the presence of impulsivity, impaired decision-making, and reward dysfunction could impact on OCD and GD patients.
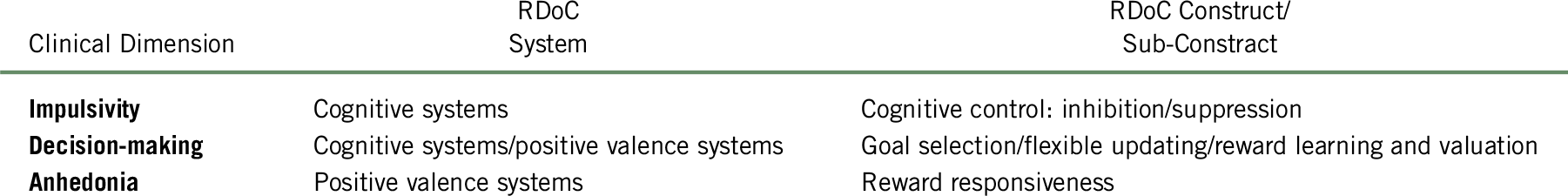
Our results could be relevant in moving forward the current OCD models, mainly focused on anxiety and compulsivity, highlighting the relevance on other RDoC dimensions such as inhibitory control networks (impulsivity), decision-making processes, and reward system dysfunctions, as putative treatment targets for OCD. Indeed, our results are in line with several neuromodulation studies that in the past years targeted these networks and showed promising results. For instance, deep brain stimulation of the reward system (targeting the nucleus accumbens and the ventral internal capsule) showed promising results in several studies,Reference Denys, Mantione and Figee42, Reference Figee, Luigjes and Smolders43 and transcranic magnetic stimulation of inhibitory control networks (targeting the supplementary motor area) also showed promising resultsReference Pallanti, Marras and Grassi44–Reference Pallanti and Hollander46 (in Figure 1 are presented the anatomical targets for neuromodulation of decision-making, impulsivity, and reward networks in OCD; in Table 3 are presented the RDoC dimensions and constructs investigated in the study).

FIGURE 1. Anatomical targeting of impulsivity, decision-making, and reward networks in OCD.
Abbreviations: ACC: anterior cingulate cortex; aINS: anterior insular cortex; BA: Brodmann’s area; CoA: cortical amygdala; DLPFC: dorsolateral prefrontal cortex; EC: enthorinal cortex; NAc: nucleus accumbens; OFC: orbitofrontal cortex; SMA: supplementary motor area; TP: temporopolar area. Brain areas involved in the same networks are grouped together. Different colors indicate different neuromodulation targets. The arrows indicate connections between brain networks
TABLE 3. RDoC systems and constructs of impulsivity, decision-making, and anhedonia in OCD
Conclusion
In conclusion, OCD patients showed several similarities and some differences compared to GD patients as well as with HCs on impulsivity, decision-making, and reward system, the three core dimensions of addiction. These results could have relevant implication for the search of new treatment targets for OCD and thus deserve further investigation.
Disclosures
The authors declare that they have nothing to disclose.